Get Advanced Insights on Any Topic
Discover Trends 12+ Months Before Everyone Else
How We Find Trends Before They Take Off
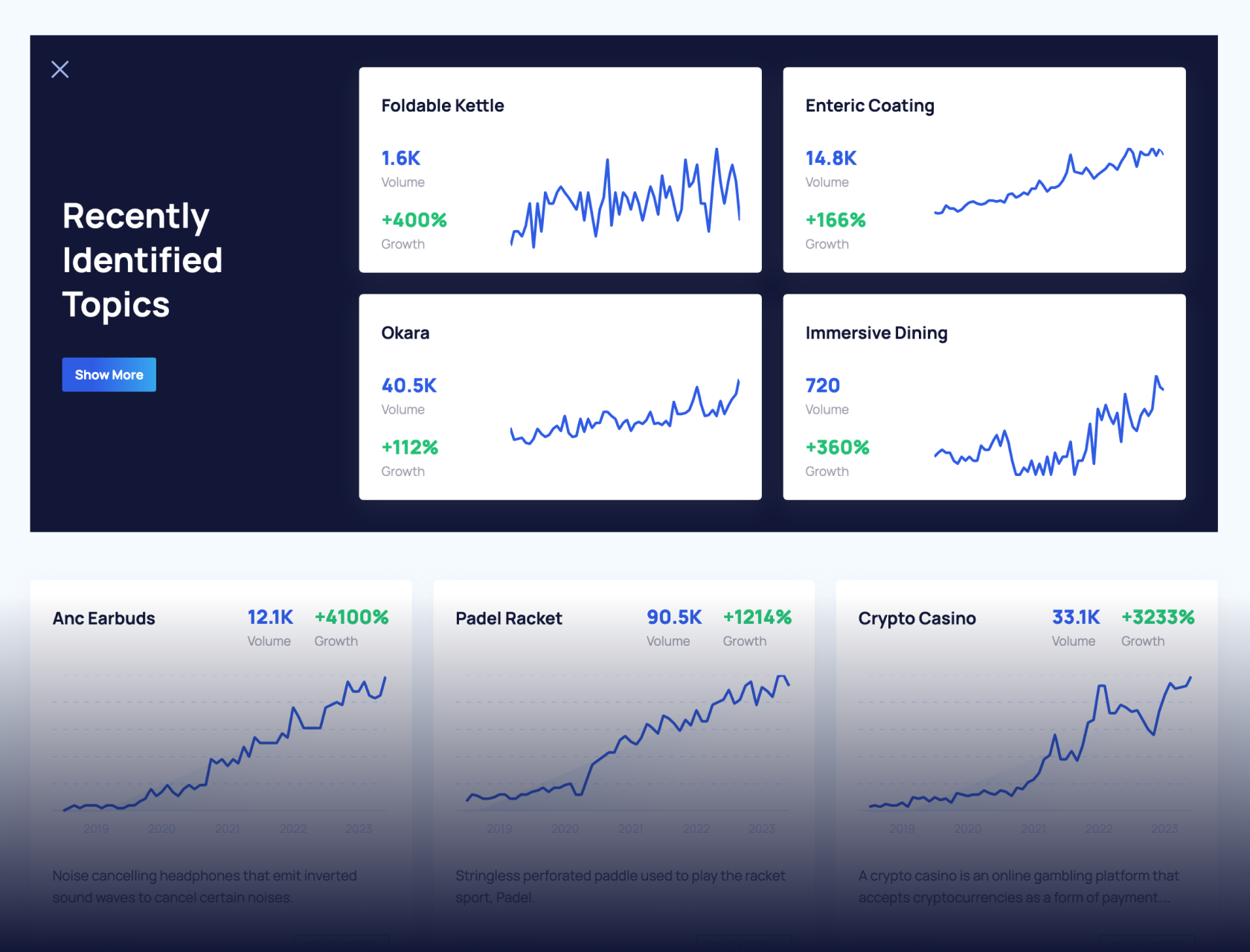
Exploding Topics’ advanced algorithm monitors millions of unstructured data points to spot trends early on.

Keyword Research
Performance Tracking
Competitor Intelligence
Fix Your Site’s SEO Issues in 30 Seconds
Find technical issues blocking search visibility. Get prioritized, actionable fixes in seconds.
Powered by data from
Future of Healthcare (2024-2027)
AI, the IoT, and 3D printing are all driving important changes to the healthcare space. Industry experts say these emerging technologies could dramatically improve patient outcomes.
However, because many communities don’t have access to any of these advancements, many groups in the industry are also calling for future priorities focused on health disparities.
In this article, we’ll outline 6 trends for the future of the healthcare space.
1. Healthcare Fully Embraces AI
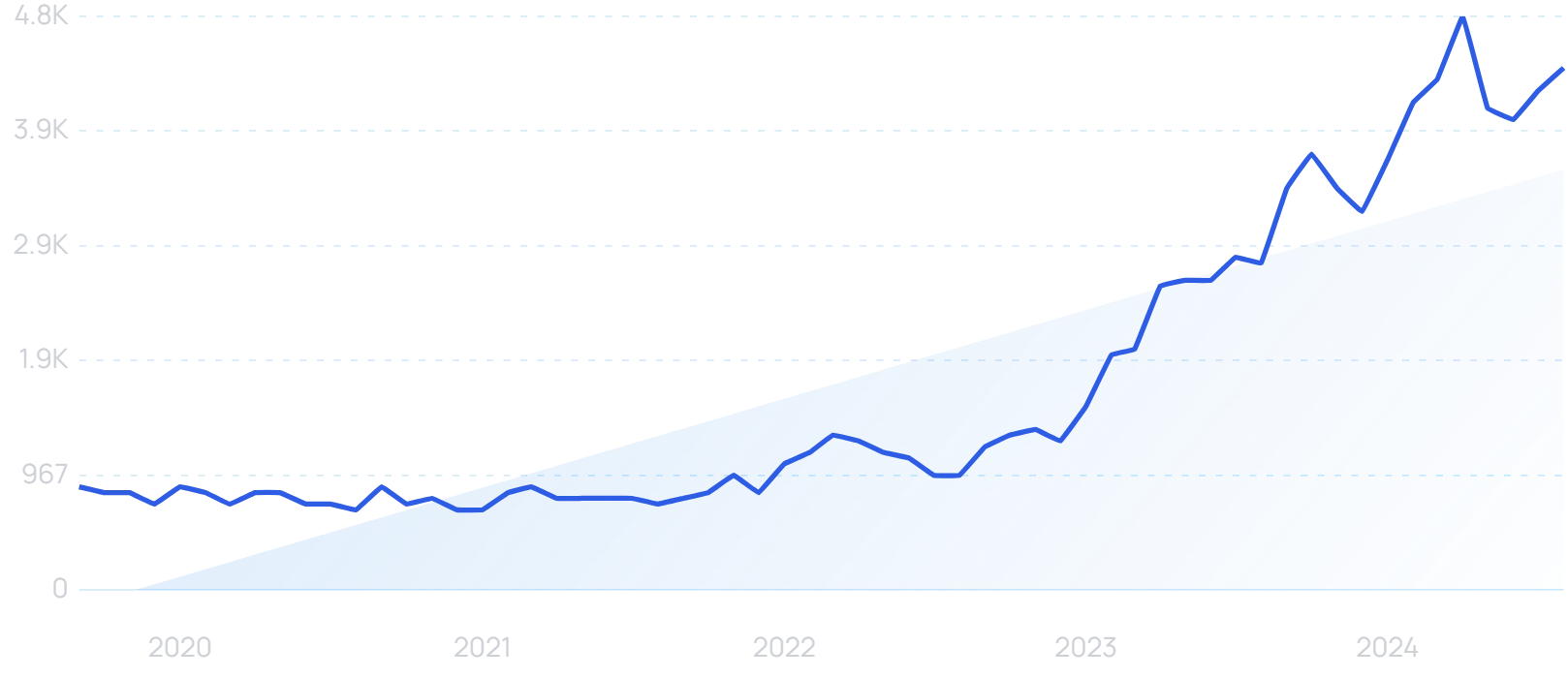
Healthcare professionals are ready to embrace artificial intelligence.
In the UK, 76% of health service staff support the use of AI in patient care, compared to 54% of the general public.
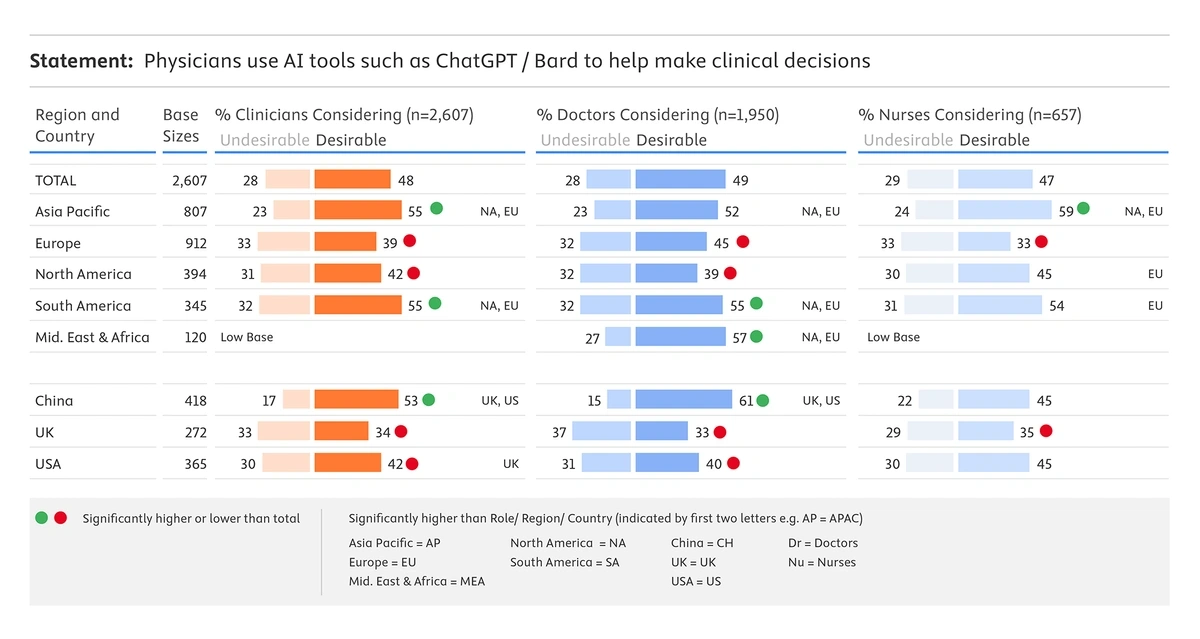
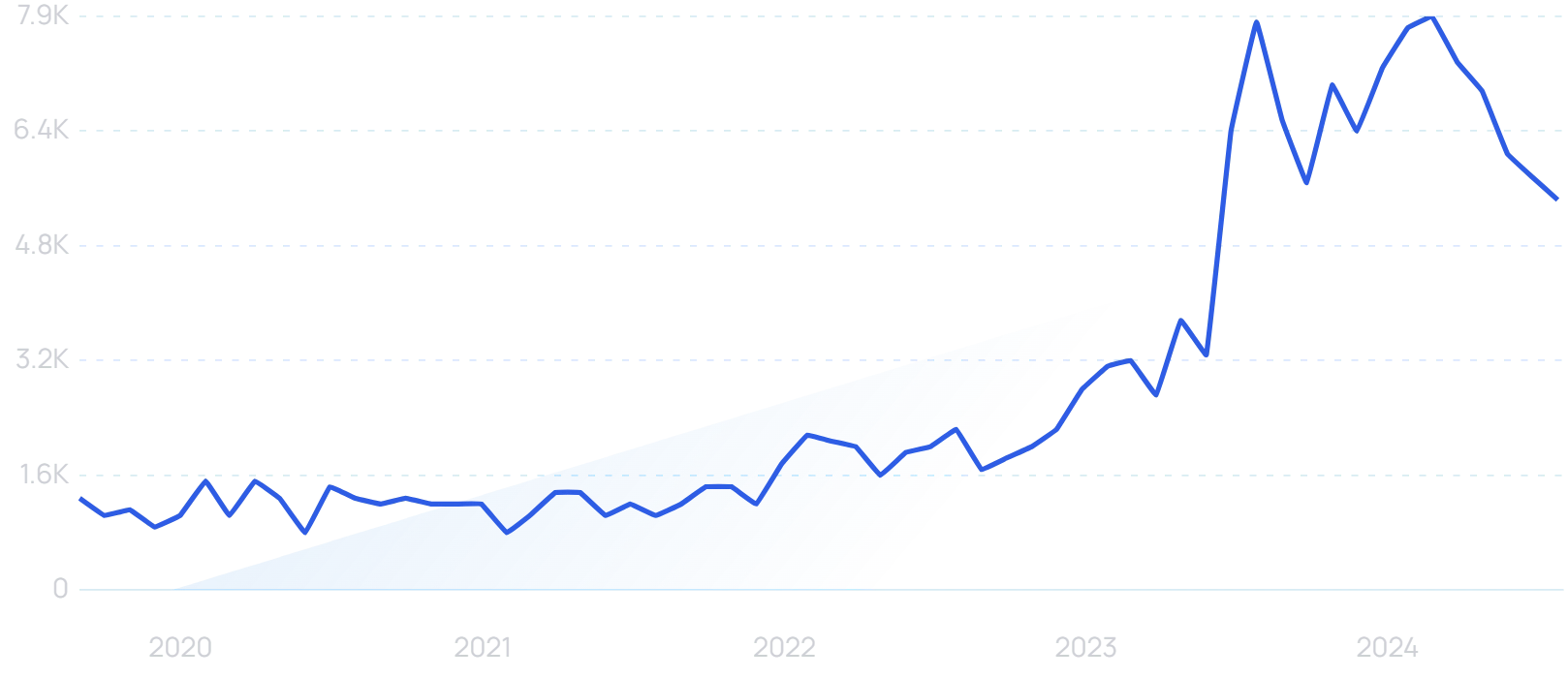
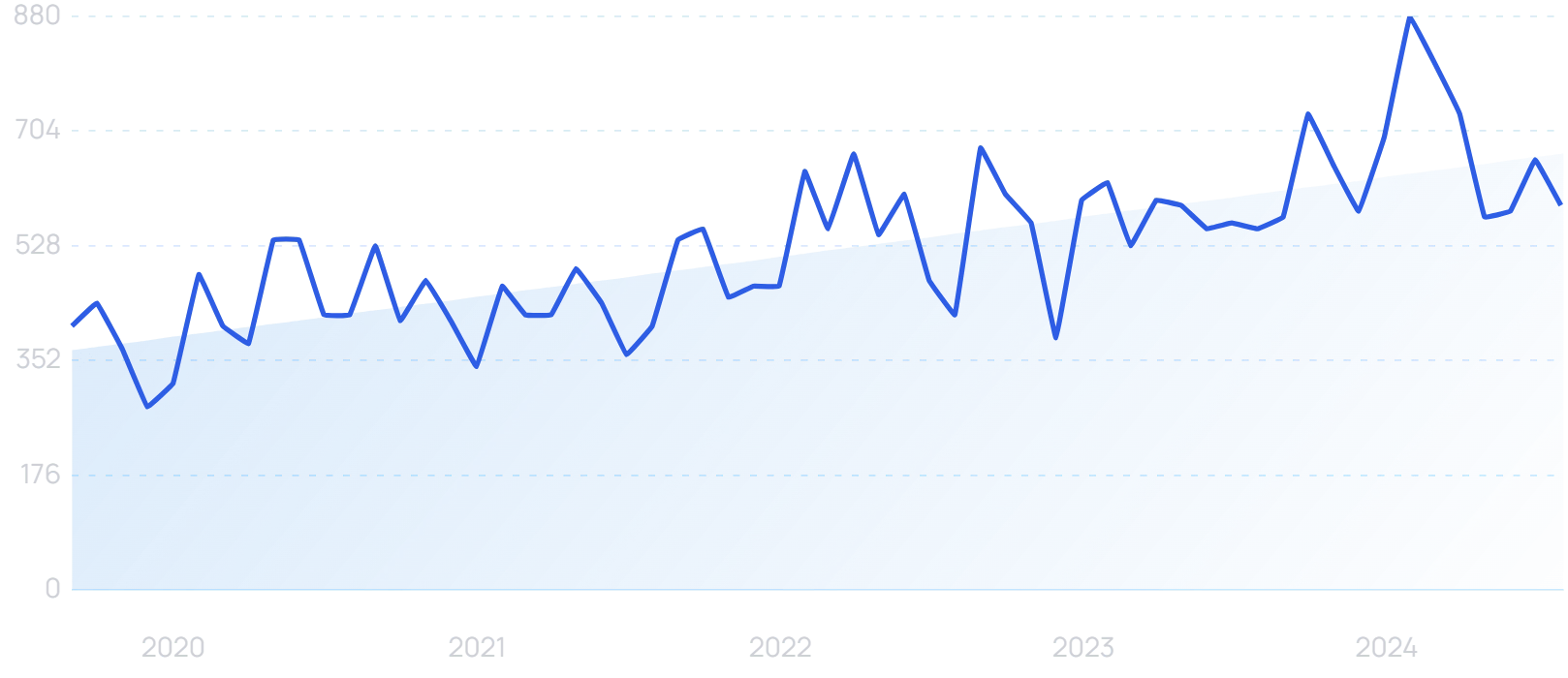
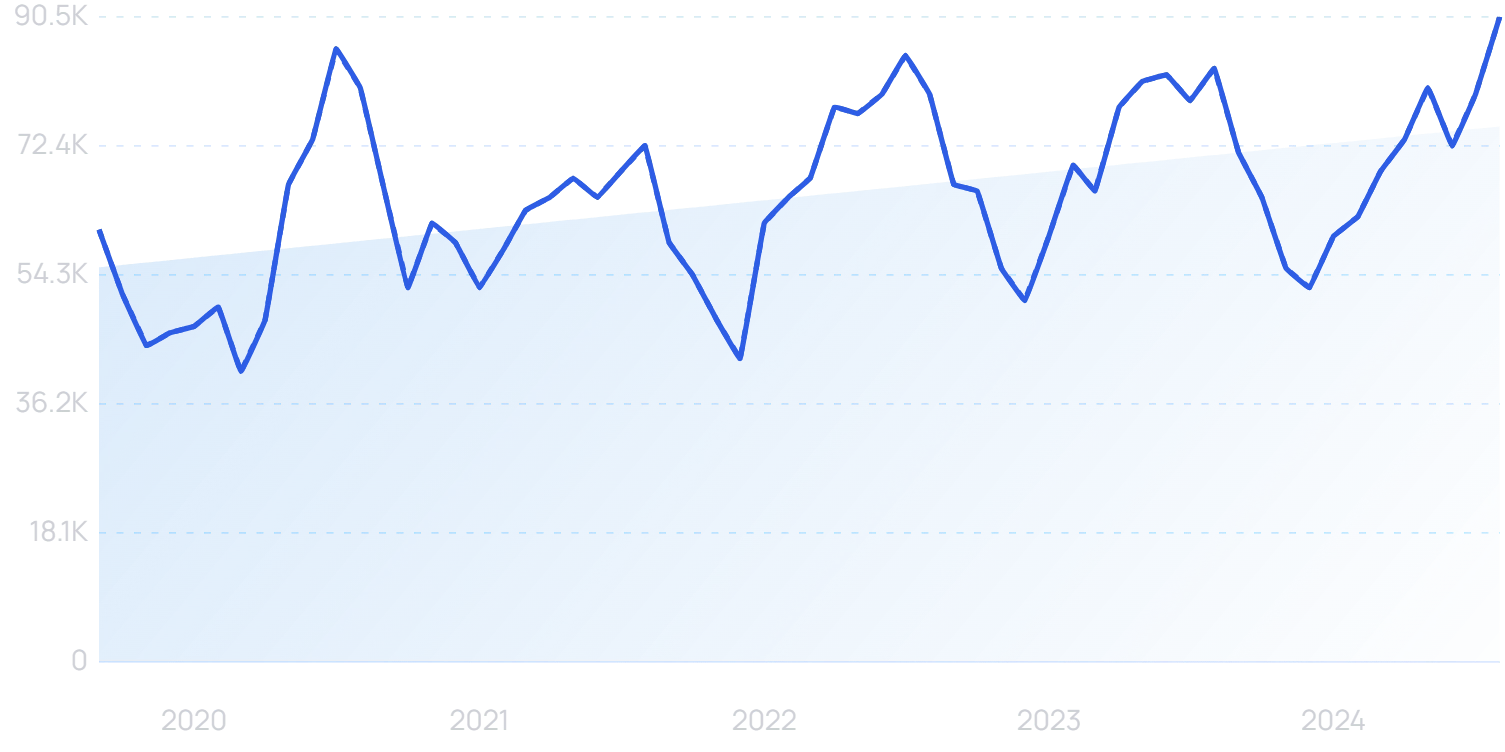
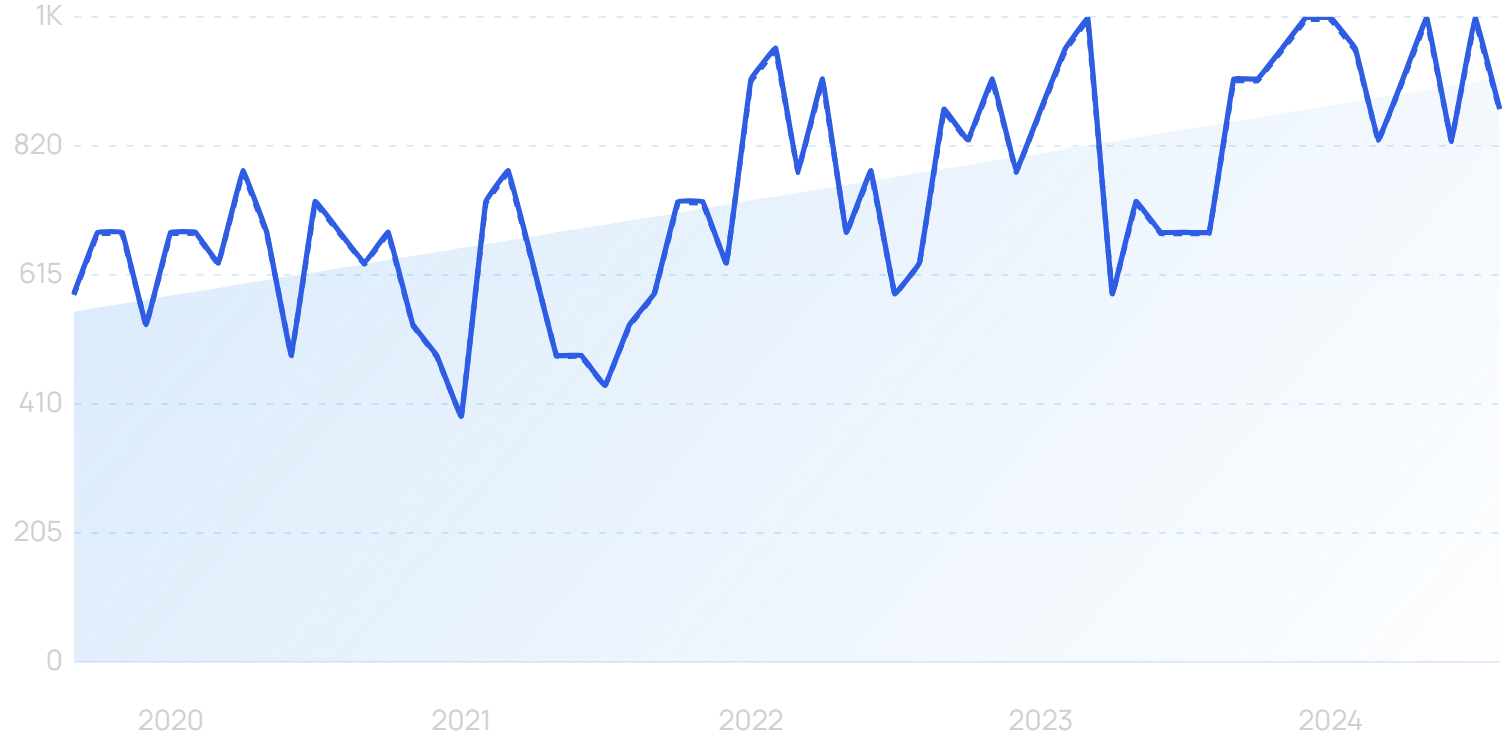
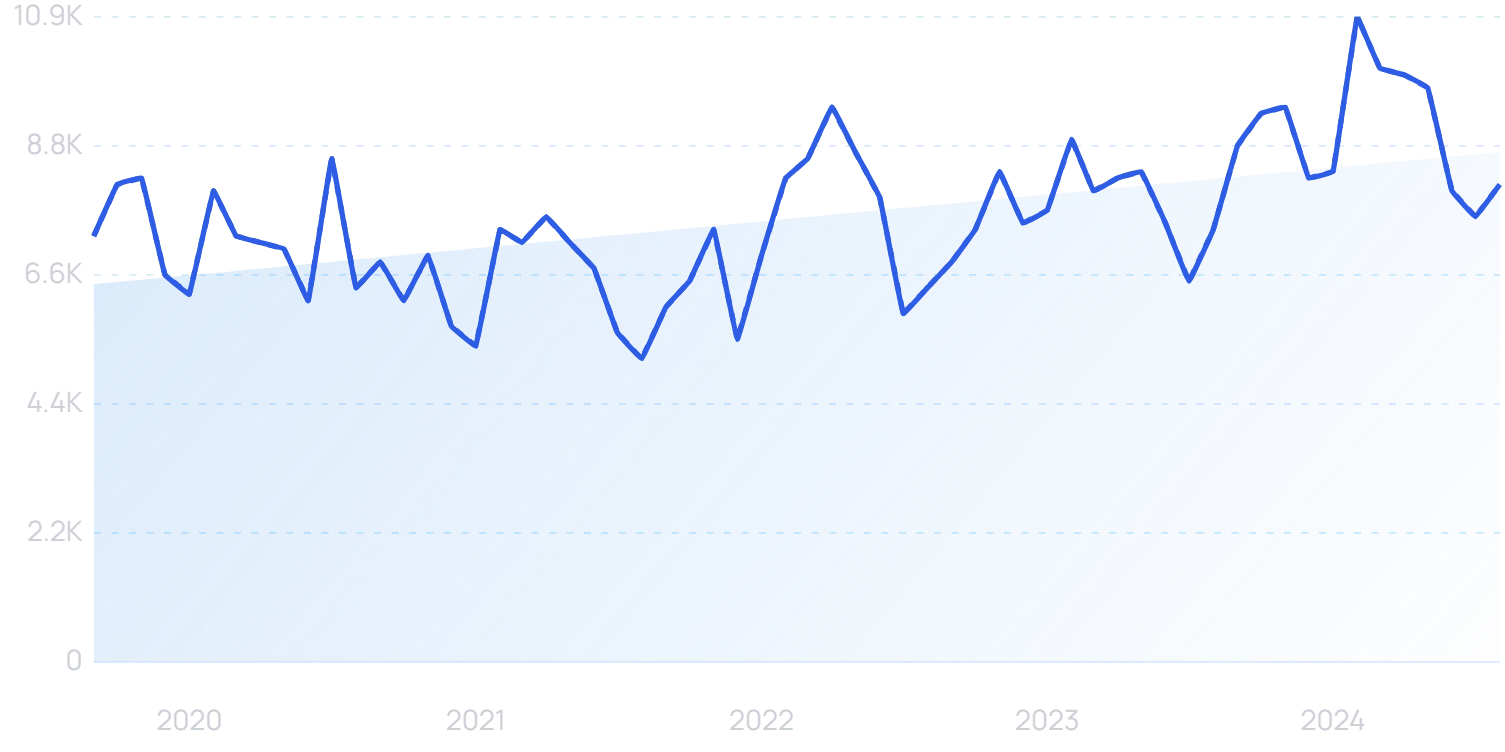
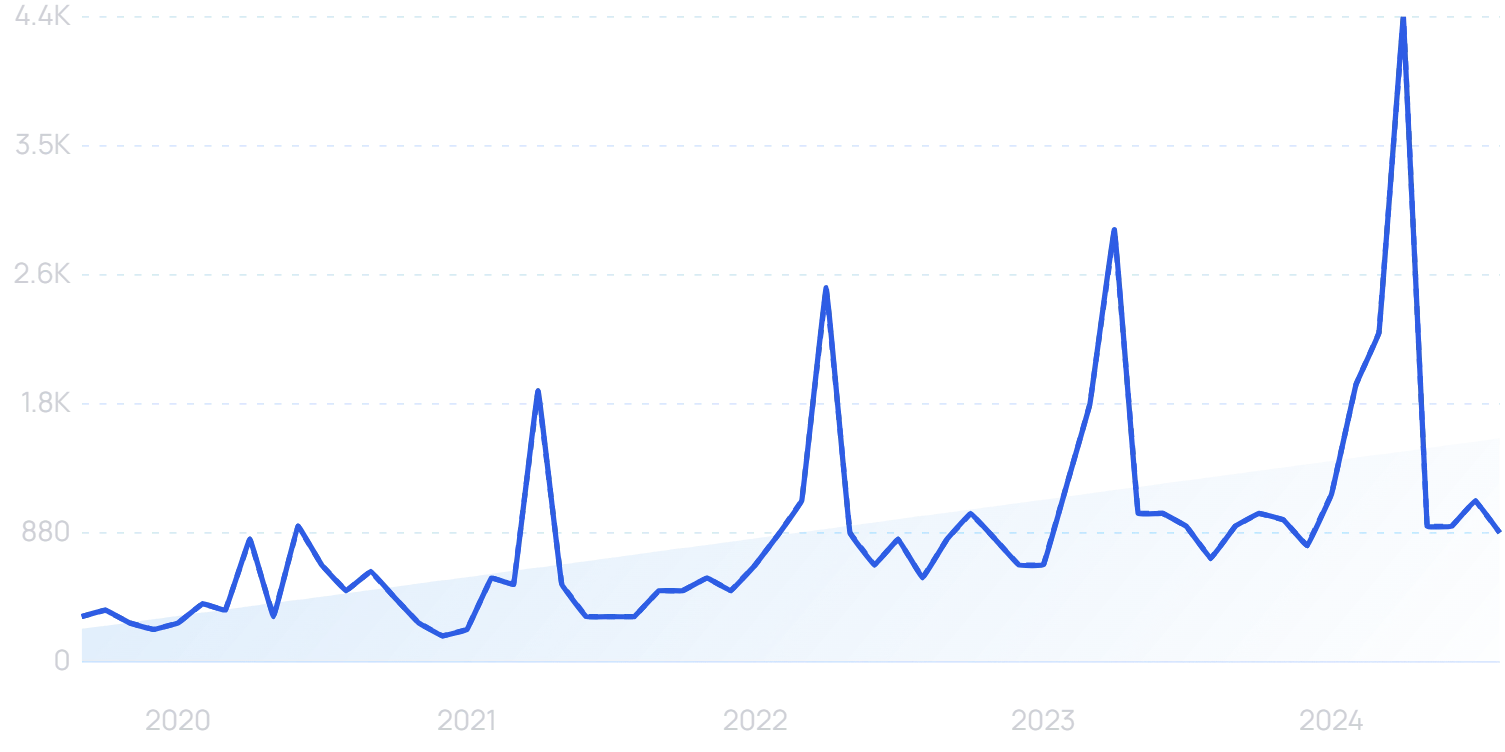
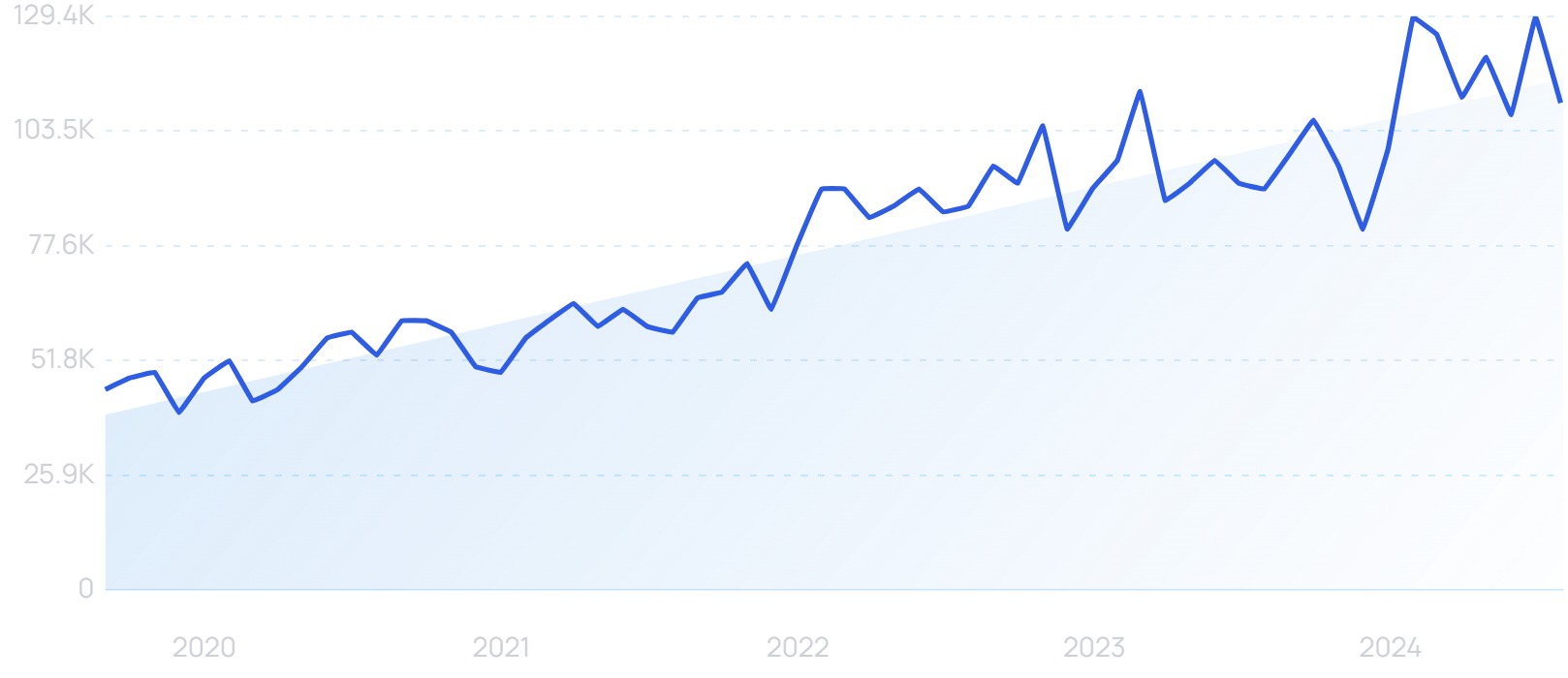
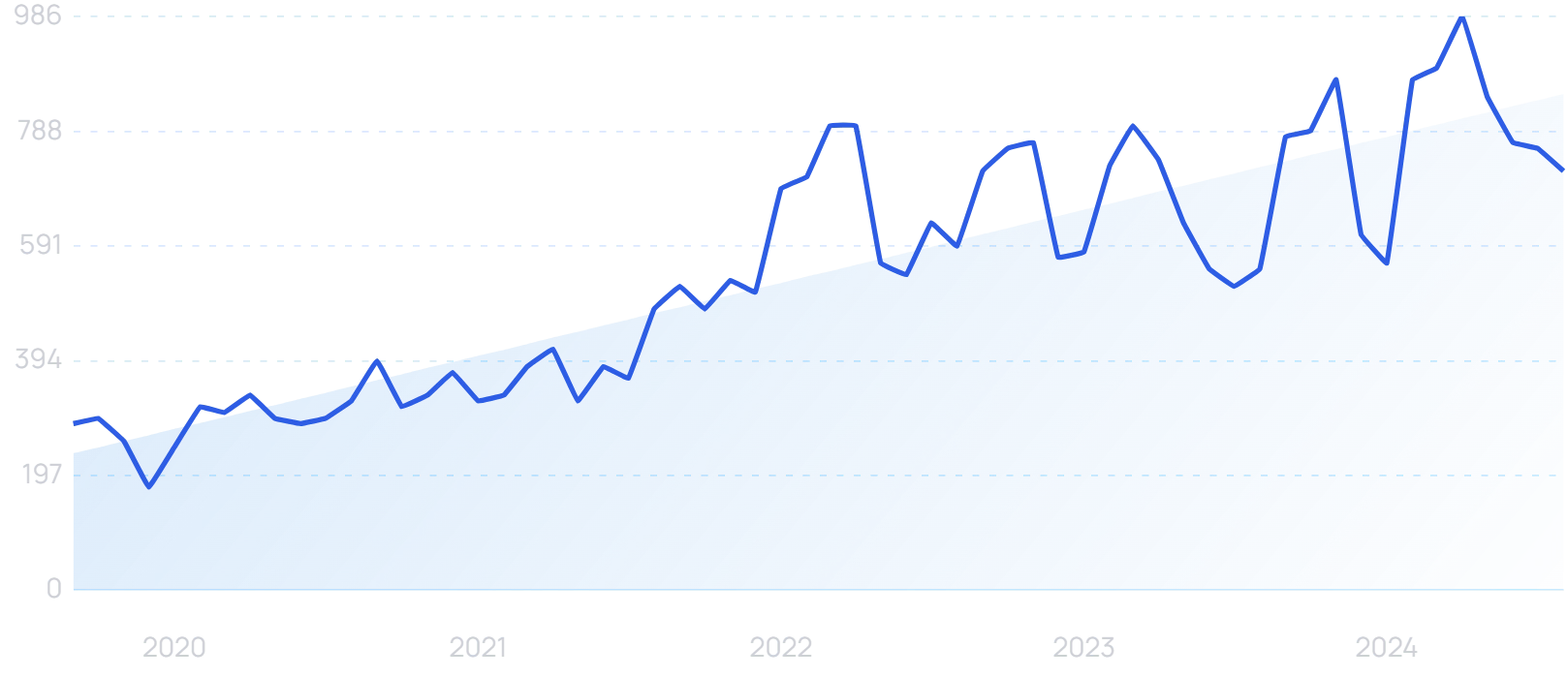
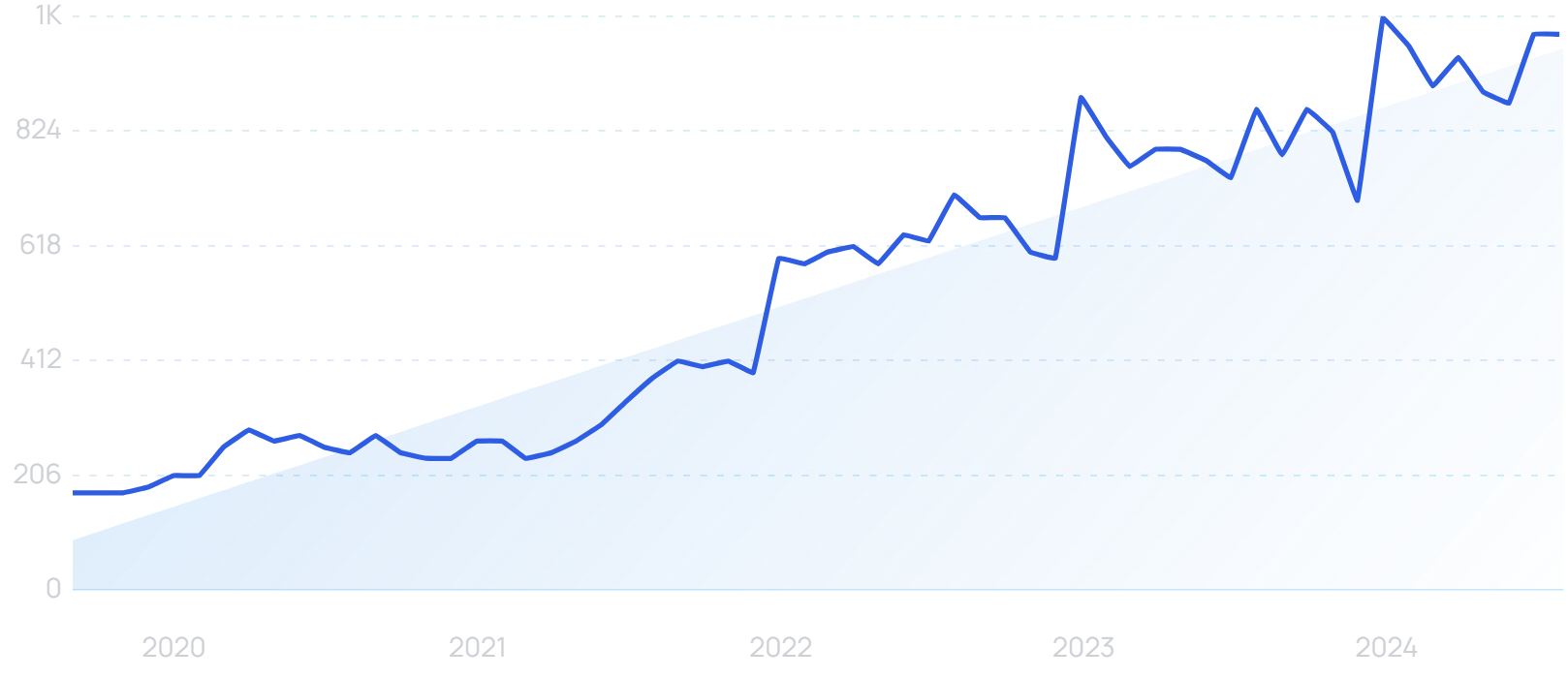
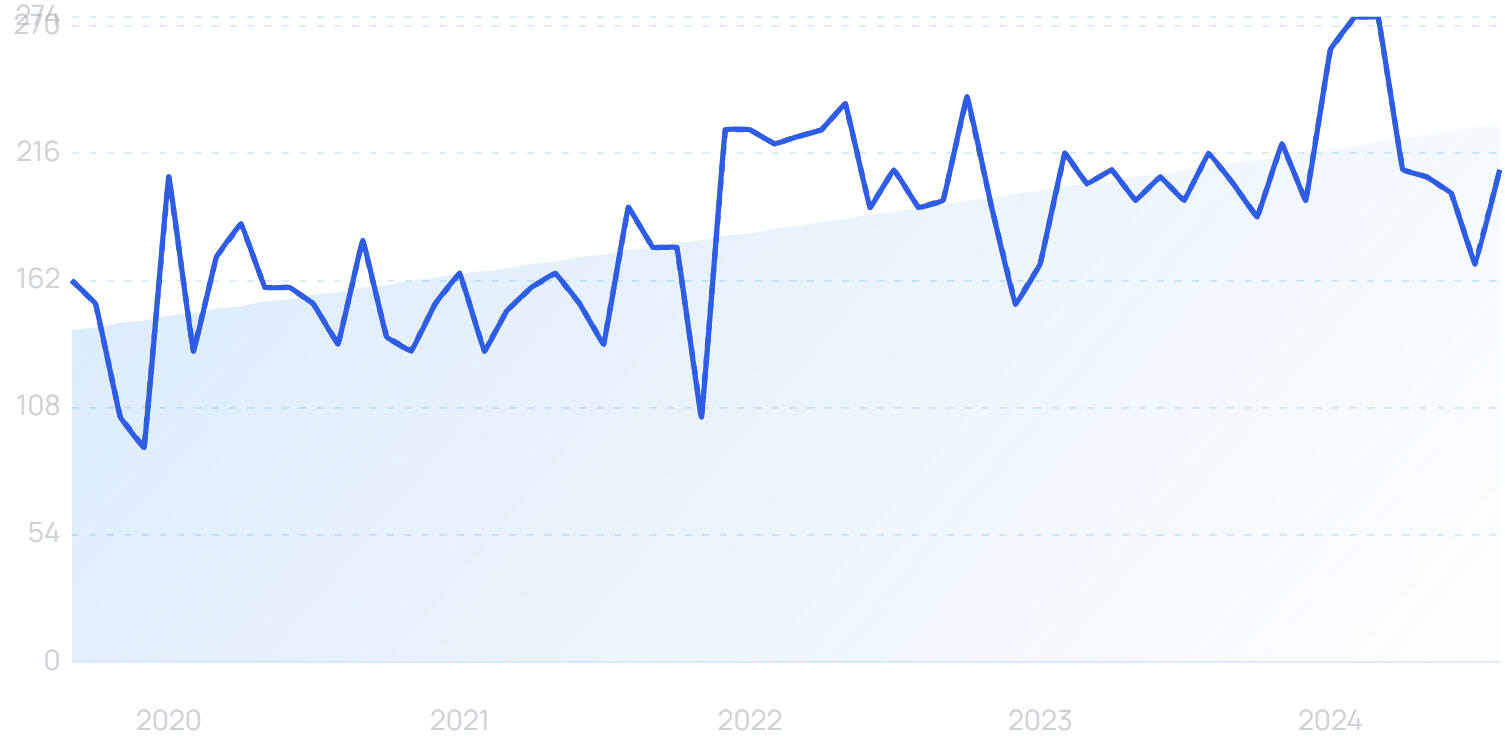
Search interest in “healthcare AI” has grown by 500% in 5 years.
There is some hesitancy among the US public. While 64% support the use of AI for managing and booking appointments, just 24% would want to see AI used for an initial primary care consultation.
Overall, however, healthcare is the area where the US public are most convinced of the benefits of AI.
And US practitioners are open to using AI in medical decision-making. 40% of doctors and 45% of nurses consider it desirable that the technology assists with clinical decisions within the next two to three years.
Clinical attitudes to AI in healthcare are especially positive in South America and the Asia Pacific region.
It’s estimated that 28% of the work done within healthcare could be automated by AI in the US and Europe.
As of November 2025, AI healthcare platform Doctronic features in the top 5 fastest-growing health startups.
In early-adopting organizations, AI solutions are already being tested in a variety of ways.
Epic, a billion-dollar healthcare software company, has more than 60 “significant” AI development projects underway.
One major use case that is already live in production gives physicians the option to use AI to auto-generate messages to patients.
CEO Judy Faulkner says clinicians and patients have actually preferred the AI responses, finding them to be more empathetic.
Some healthcare startups are looking to take generative AI even further in the coming years.
Hippocratic AI is creating a large language model that company officials hope will improve access to healthcare and positive outcomes from treatment.
However, they have distinctly noted that their platform is not aimed at making diagnoses.
Instead, leaders say it will have the potential to explain billing to patients, remind patients to take medication, answer pre-op questions, and deliver test results.
Leaders also stress that they’re building the platform with a focus on safety and are committed to delaying its release until it’s been tested and approved by a large number of healthcare professionals.
It’s currently being tested by more than 5000 nurses and 500 doctors.
Hippocratic is into its third phase of safety testing.
As for the use of AI in a clinical setting, a University of California study has found an application in the context of triage.
It used ChatGPT-4 rather than any kind of specialized AI.
Even so, when faced with two sets of patient symptoms, the AI correctly identified the more urgent condition in 88% of cases. Physicians were right 86% of the time.
Aidoc uses a purpose-built medical AI platform to achieve similar goals.
Searches for “Aidoc” are up by 146% in 5 years.
It analyzes 3 million patients every month. Its technology is live in more than 1000 medical centers.
AI is also beginning to be implemented in order to follow up with patients even when they’re not in the hospital or medical facility.
Ufonia, an Oxford-based business, has developed the first AI-powered clinical assistant approved for marketing in the UK.
“Dora” has already been used to follow up with patients who have had cataract surgery, making automated phone calls in place of routine interactions with healthcare staff.
“Dora” can conduct voice conversations with patients in a variety of languages.
Using the technology in an orthopedic setting, the University of Leicester reduced the backlog of patients waiting by 11%.
Drug discovery is also an area where AI could prove to be completely transformative.
“AI drug discovery” searches are up 325% in 5 years.
Combating an average expenditure of $1 billion to bring a drug to final approval, AI such as Google’s AlphaFold can predict how molecules and proteins will react.
Ultimately, it could reduce the amount of trial-and-error involved in discovering new drugs, vastly streamlining the process.
In the coming years, healthcare tech companies are likely to continue to expand upon these example use cases and look for ways to make AI even more impactful in the healthcare sector.
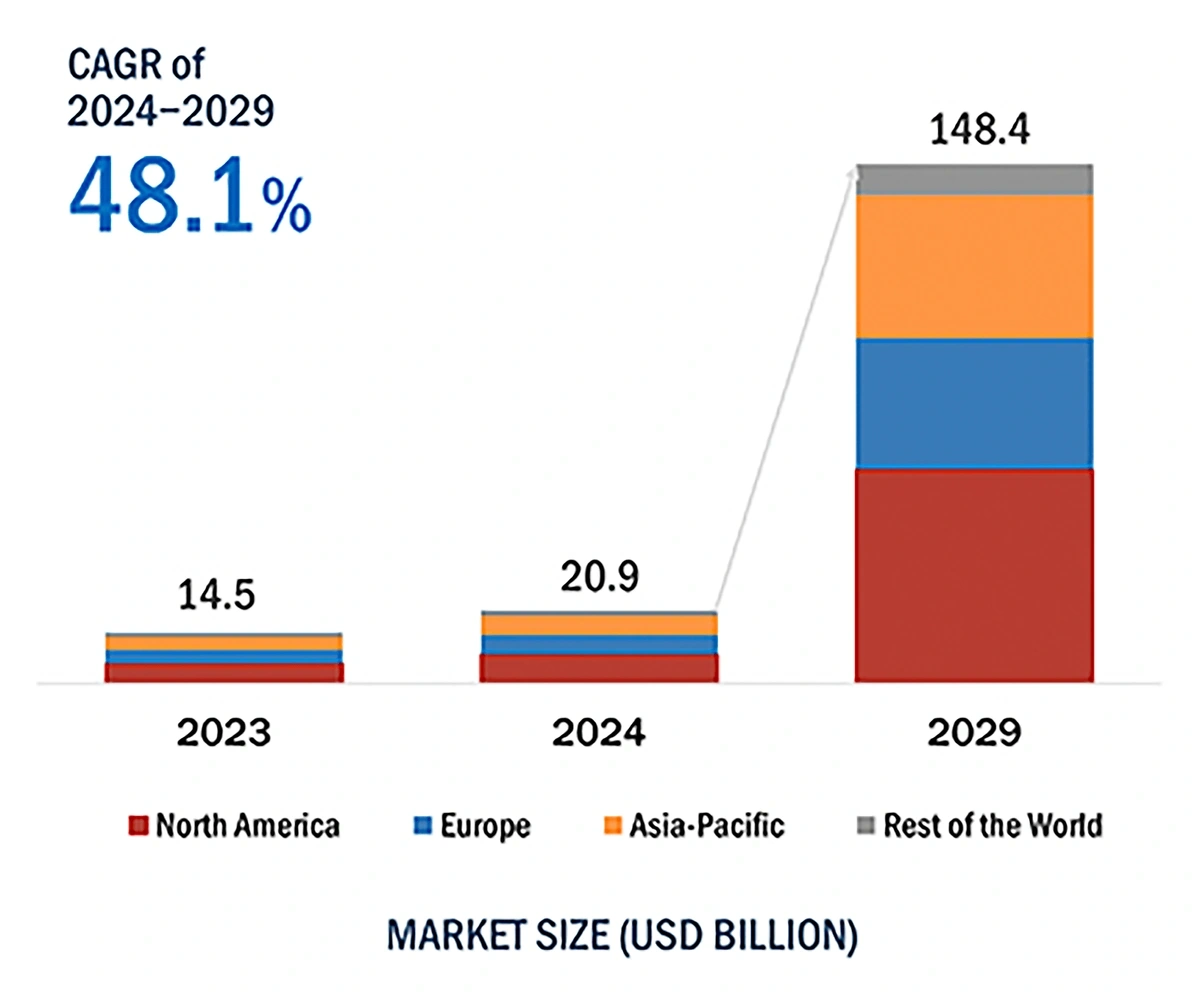
Predictions show the market value of AI in healthcare could soar as high as $148.4 billion by 2029.
The AI healthcare market was valued at around $21 billion in 2024 but could potentially add more than $125 billion in value before 2029.
2. Healthcare Data Undergoes A Revolution
More than half of healthcare organizations (51%) believe they need to modernize their data stack “a great deal” this year.
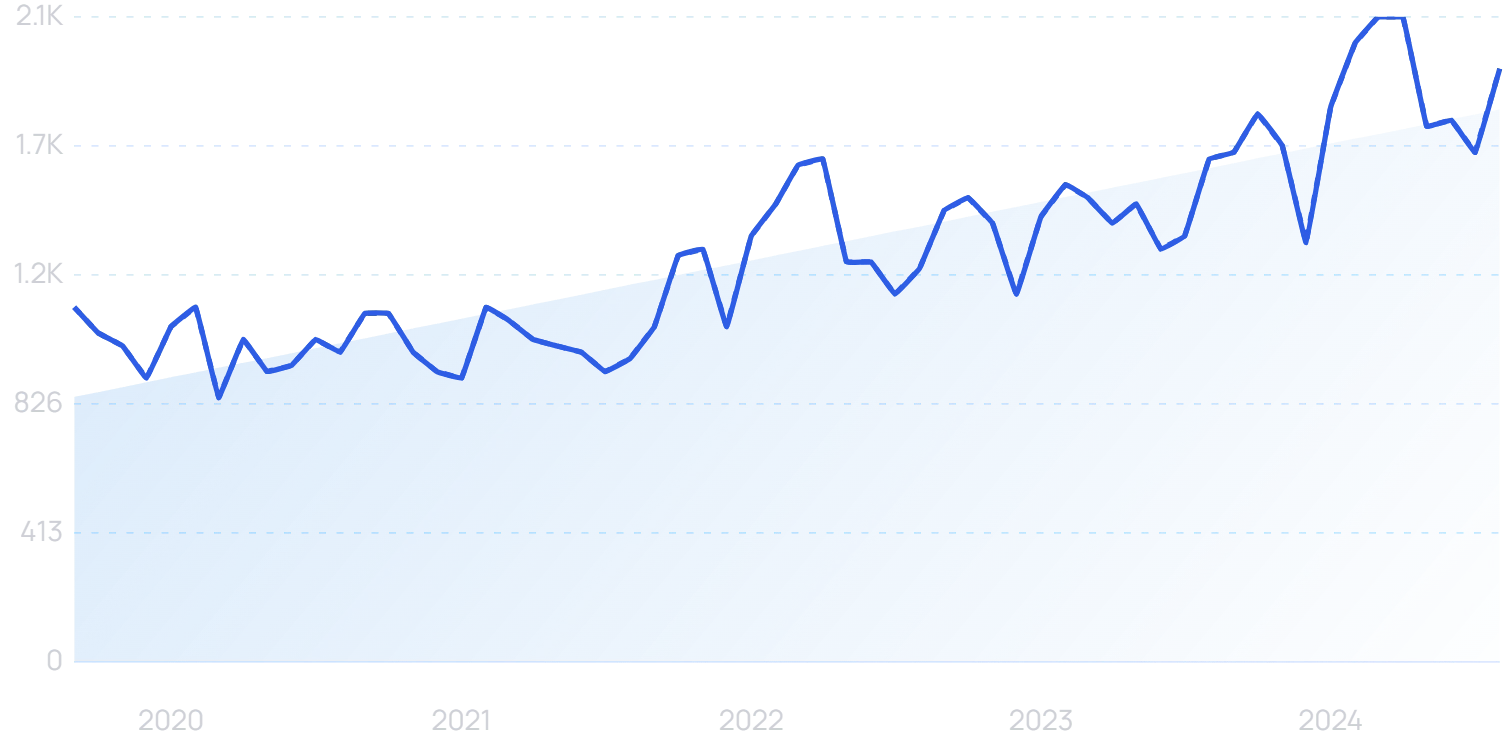
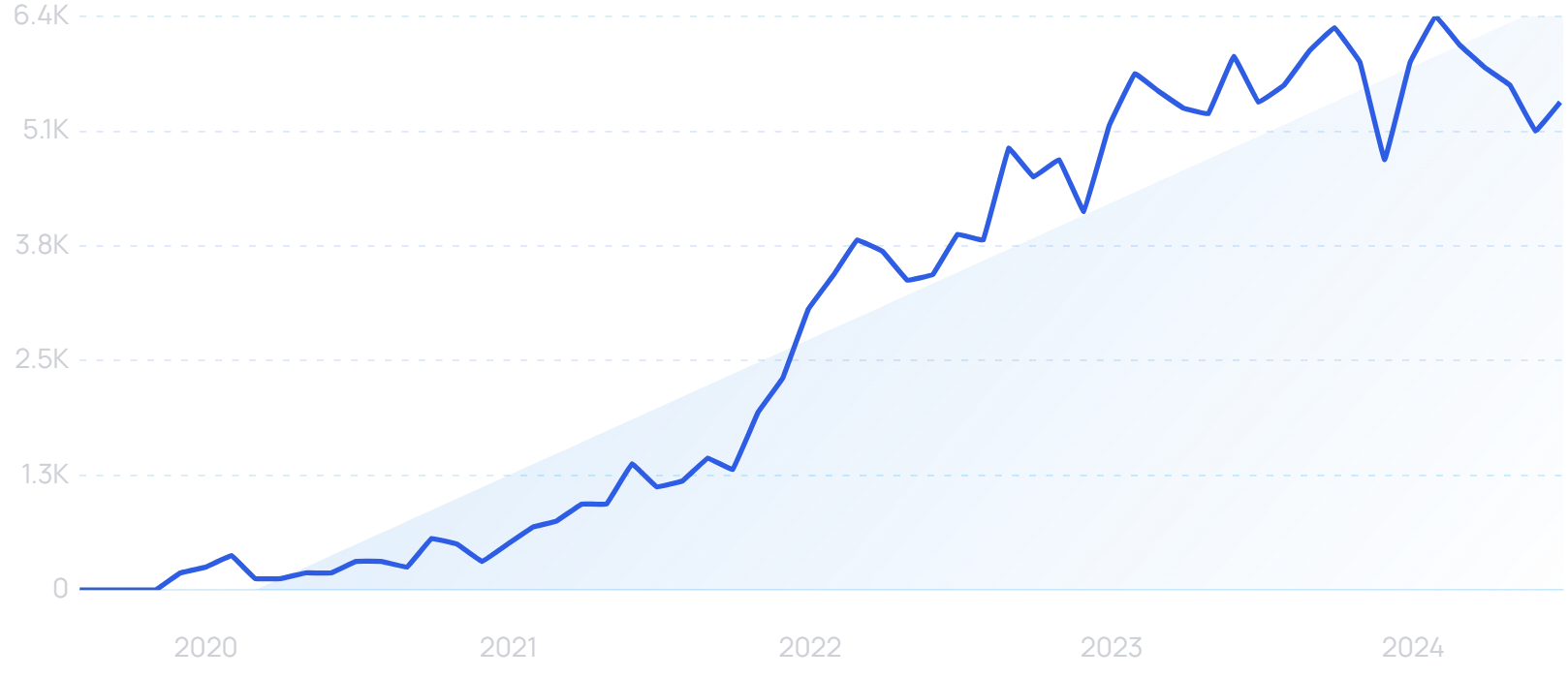
Searches for “healthcare data” are up 78% in 5 years.
Perhaps that’s no surprise.
The healthcare industry is a huge contributor to the modern data explosion, which sees more than 400 million terabytes of data created every day.
73% of clinicians now believe it is important for doctors to be digital experts. While only 61% believe they have enough time to provide good patient care.
As such, it’s more important than ever for the healthcare industry to get a firm handle on its data.
Healthcare data comes from hundreds of sources, everything from physician notes to lab results to patient feedback.
Philips reports that 94% of healthcare leaders say that their organization faces at least one data integration challenge that impacts its ability to deliver timely and high-quality patient care.
43% believe that optimizing treatment plans and care pathways can be improved through data-driven insights.
That all comes back to “healthcare interoperability” - the sharing of data between departments and organizations.
Search volume for “healthcare interoperability” has increased in recent years.
Healthcare experts see a bright future in which the entire medical ecosystem is seamlessly connected. Devices and systems could interact with each other without human intervention.
But that’s not a reality yet. Today’s data and infrastructure is still highly fragmented.
A visualization of the medical data fragmentation issue.
That’s why many healthcare organizations are moving their data to the cloud.
What was once seen as a security risk is now seen as a necessary transformation that can deliver cost savings and better patient care.
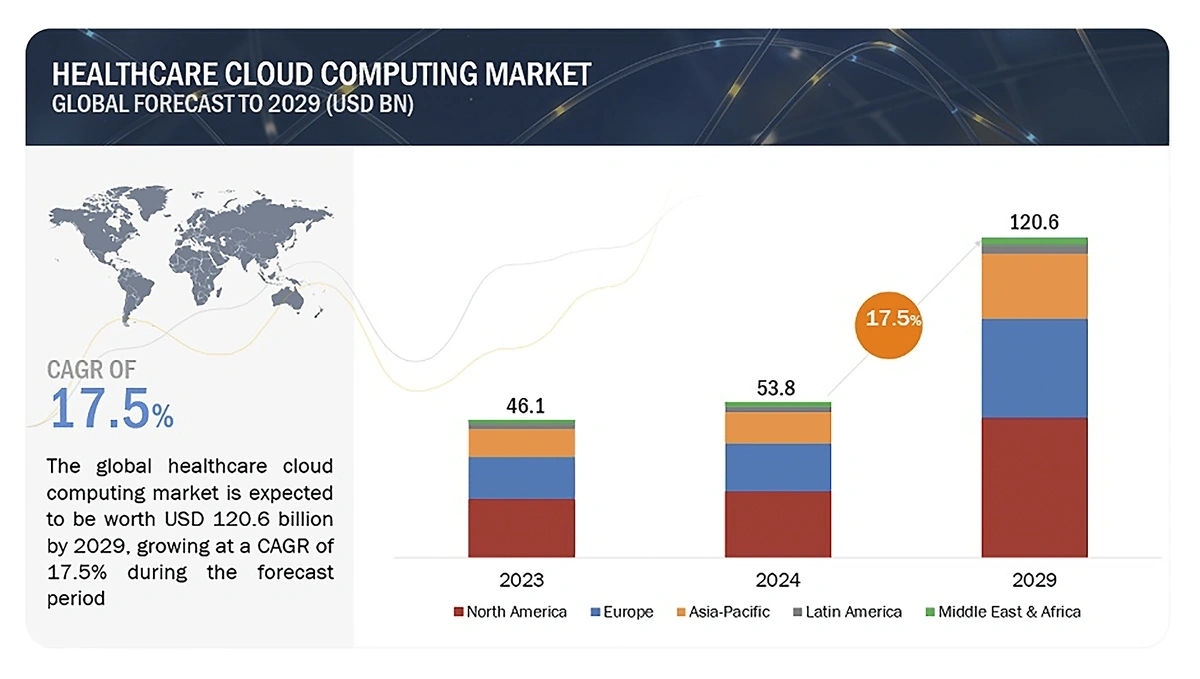
The healthcare cloud computing market is growing. It’s already worth $53.8 billion, and predictions show a 17.4% CAGR between 2024 and 2029.
The healthcare cloud computing market could be worth more than $120 billion by 2029.
Cloud storage can save healthcare organizations as much as 30% compared to traditional storage..
However, cloud providers do need to address security concerns before healthcare data can be fully transformed.
In the first half of 2024 alone, more than 31 million Americans were affected by just the top 10 biggest breaches of health data.
And data breaches in healthcare are the most costly of any industry. Last year, the average cost was $10.93 million per breach, more than double the figure for the financial sector.
Increasing cybersecurity is expected to be a critical task for health systems going forward.
At this point, most health organizations are reactive instead of proactive when it comes to protecting their IT systems and data.
Ordr is a startup cybersecurity company that specifically protects connected devices and their data in healthcare settings.
“Ordr” searches are up 45% in 5 years.
This includes medical devices, basic IoT devices like printers, and even on-premises cameras.
The company has raised $90 million in investment.
As healthcare leaders look to the future of connected care, both cloud computing and security are likely to demand increased investments.
57% of healthcare IT professionals expect their cybersecurity spending to rise this year, with only 3% forecasting a fall.
3. IoT Transforms Healthcare
Much of the data created in the healthcare sector comes from IoT devices, which is often referred to as the IoMT (Internet of Medical Things).
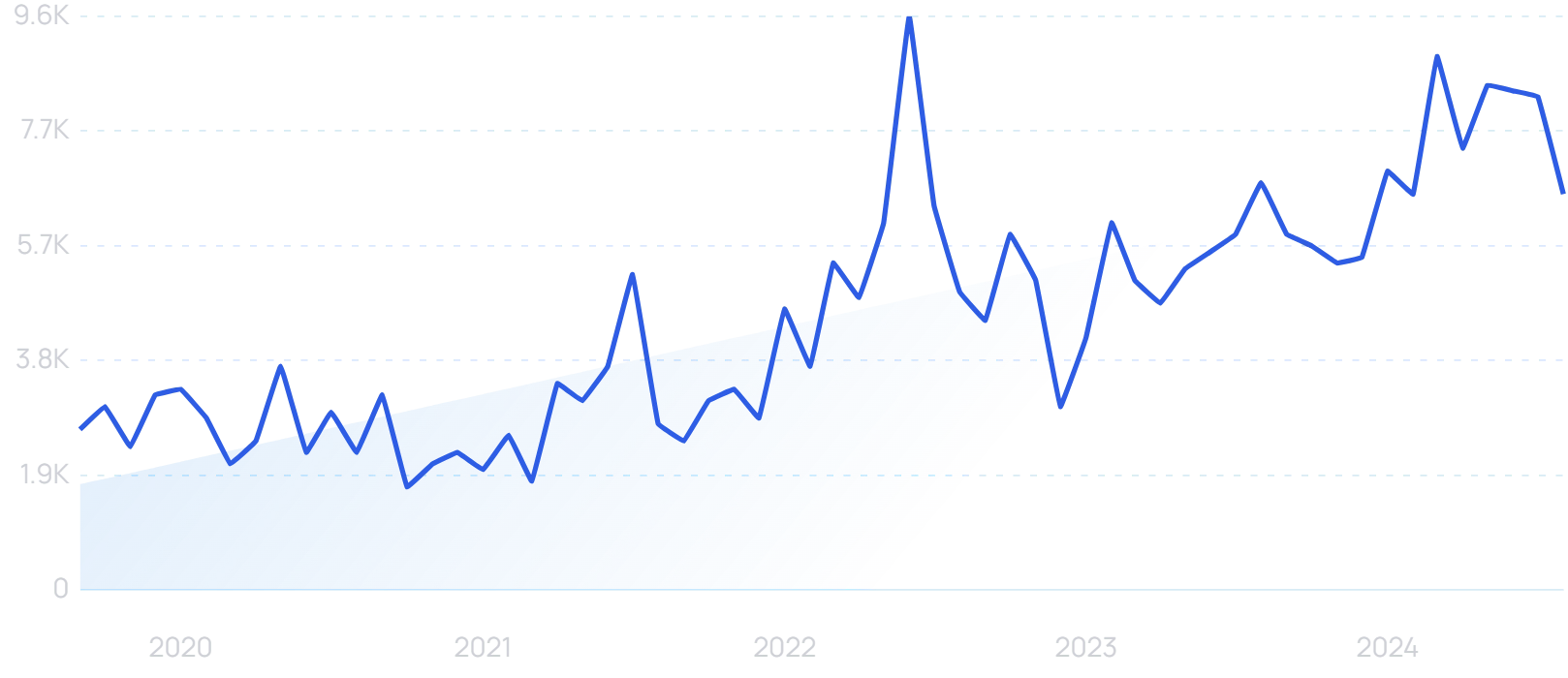
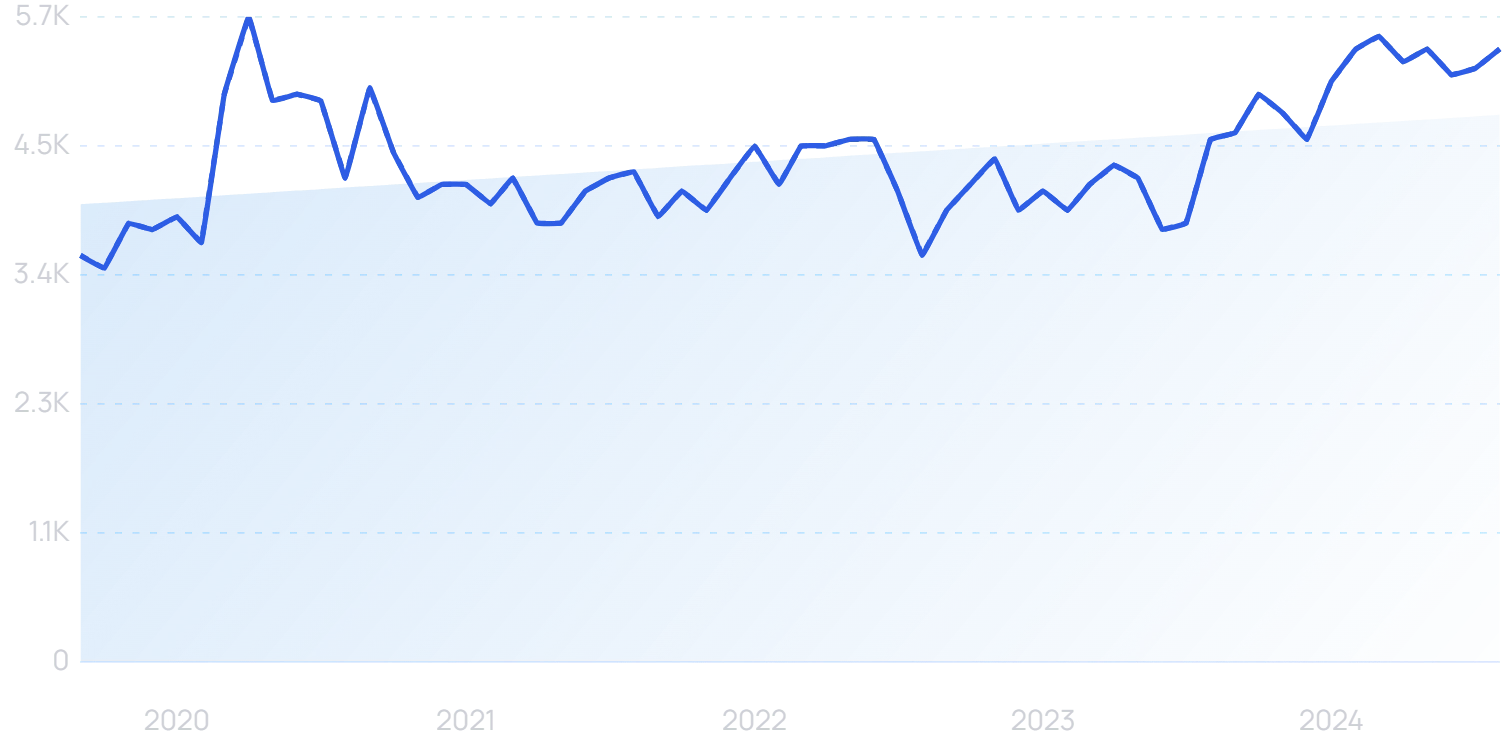
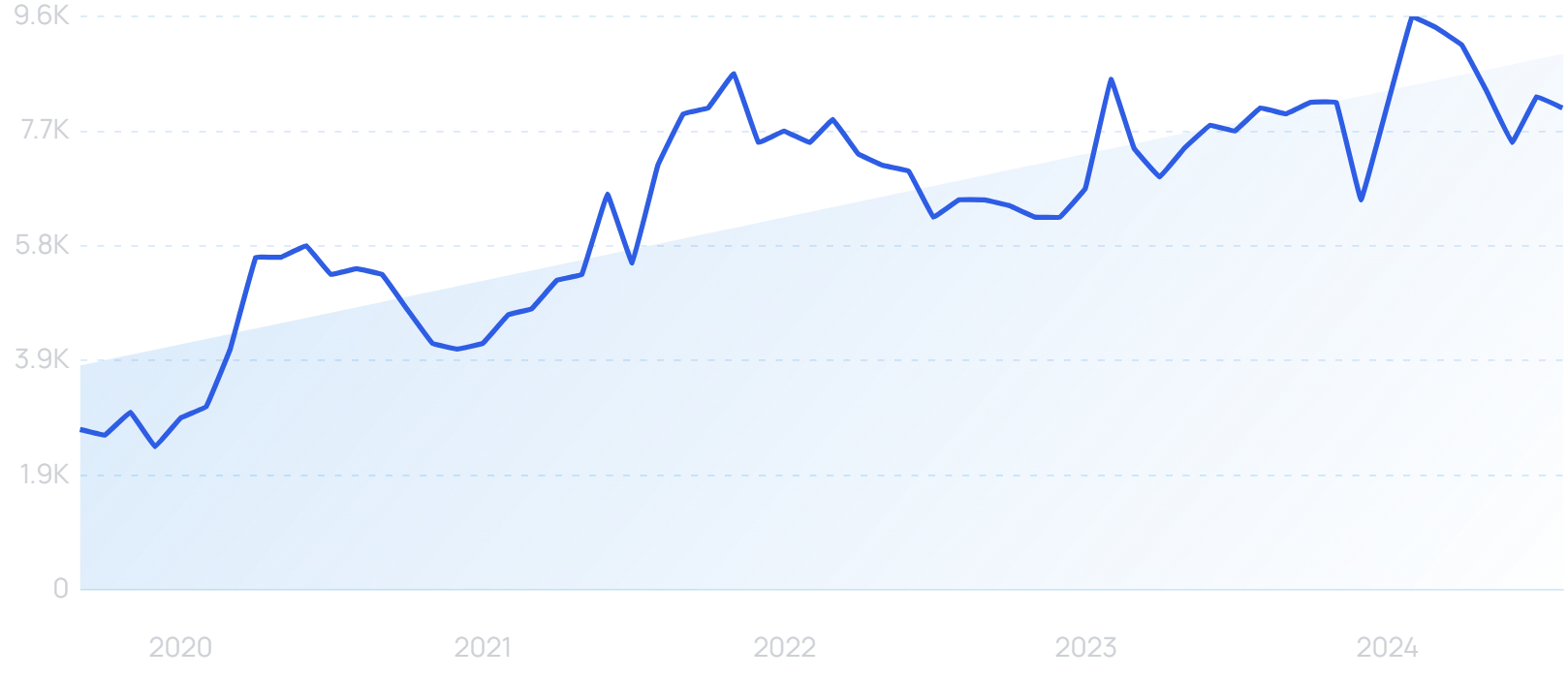
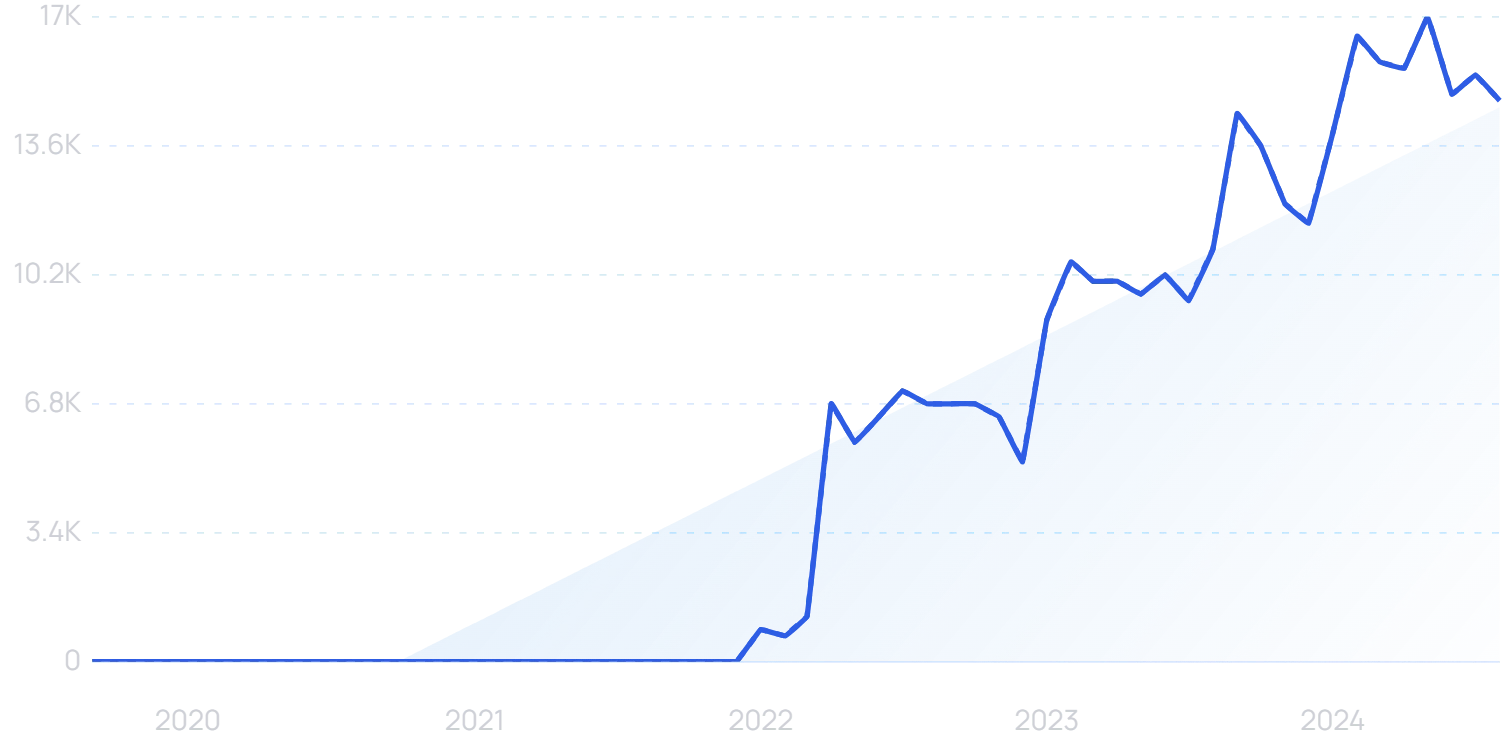
Search volume for “IoMT” has jumped by 129% in the past 5 years.
According to InsightAce Analytic, the market for IoMT is surging with a CAGR of nearly 30% projected through 2031. Its total value could reach $385 billion by that time, more than a 7x growth over last year.
Much of this growth could come from an increase in remote patient monitoring (RPM) and the devices used for that type of healthcare.
The pandemic ushered in this digitization of healthcare, and even though the pandemic is gone, patients are still demanding RPM.
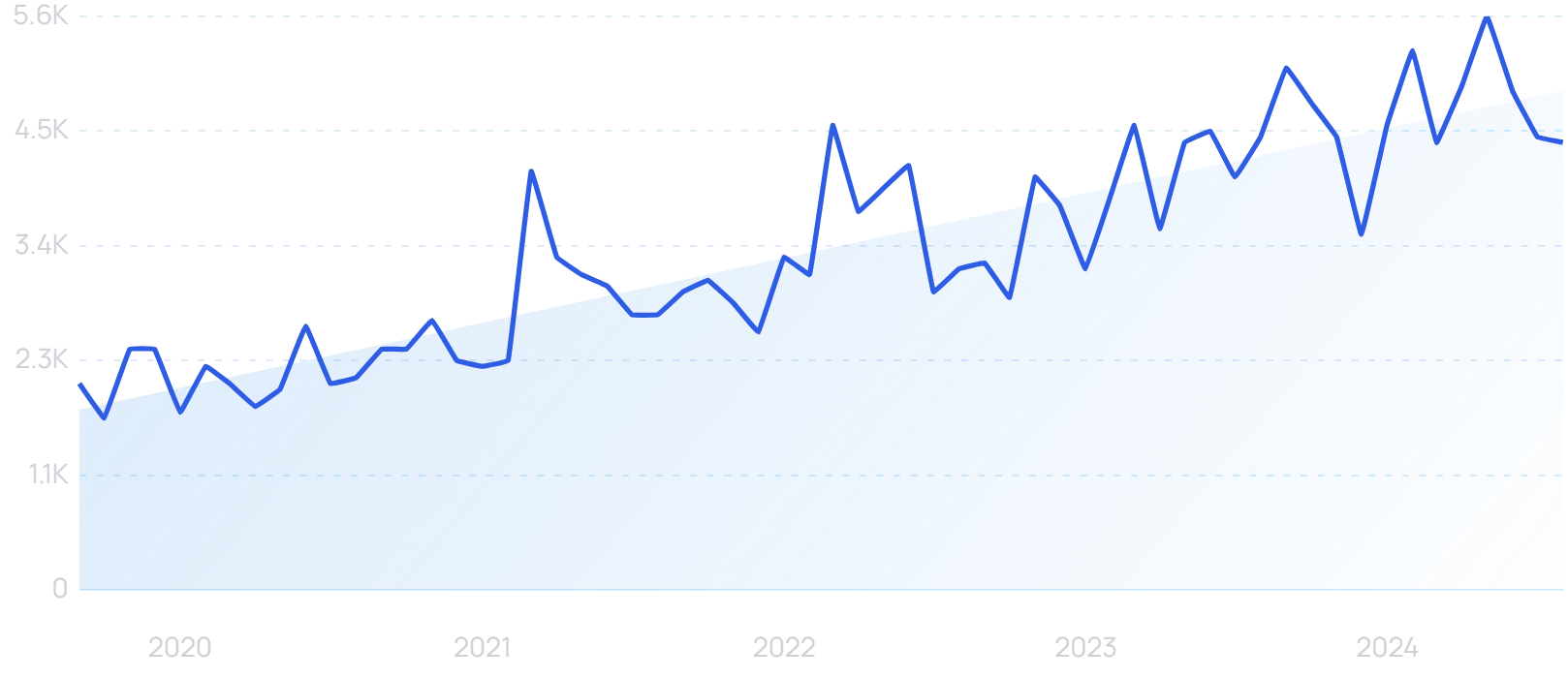
Searches for “remote patient monitoring” are up 196% in 5 years.
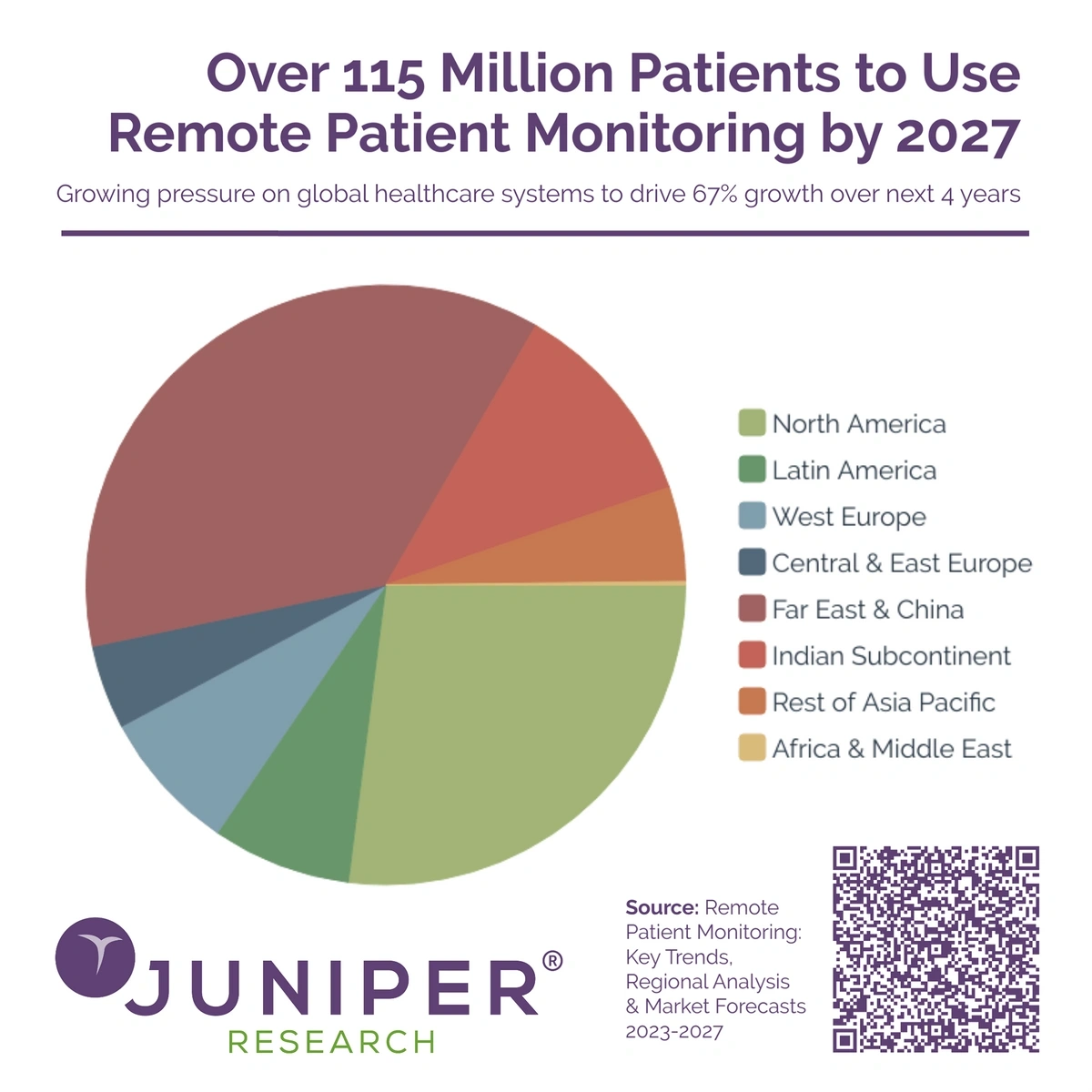
Juniper Research reports the number of RPM users could reach over 115 million by 2027.China and the Far East will account for the most users, along with North America.
75 million people used RPMs last year, a tally that could swell by more than 40 million by 2027.
When it comes to health wearables, 68% of clinicians think it is desirable for this type of patient-collected data to inform clinical decisions.
Smartwatches and fitness trackers are expected to continue to grow in popularity in the coming years.
But so are more advanced RPM devices like clinical-grade wearables.
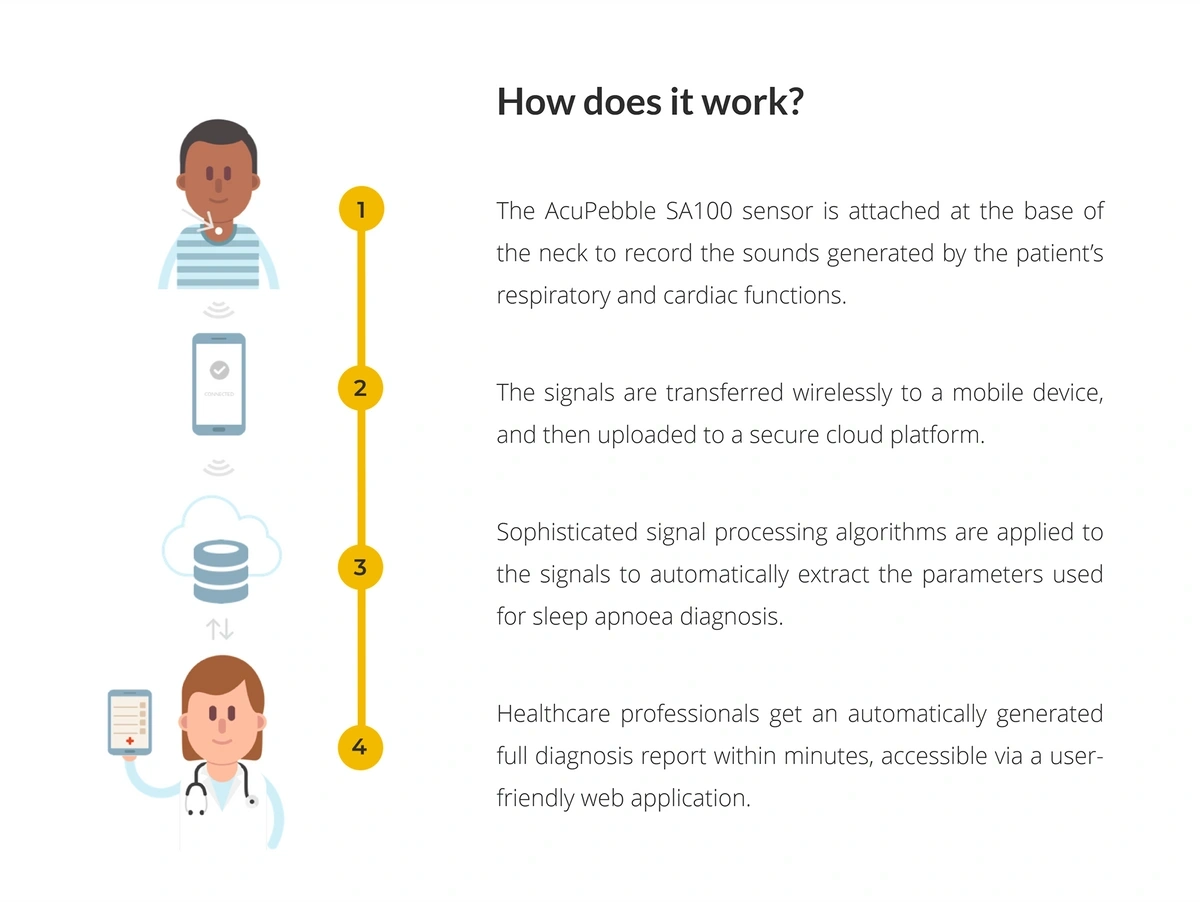
For example, Acurable has developed a wearable that can detect sleep apnea remotely.
Acurable’s device sits at the base of the neck and sends data to a cloud platform via the user’s mobile device.
In trials, the device accurately diagnosed 100% of cases of moderate and severe sleep apnea.
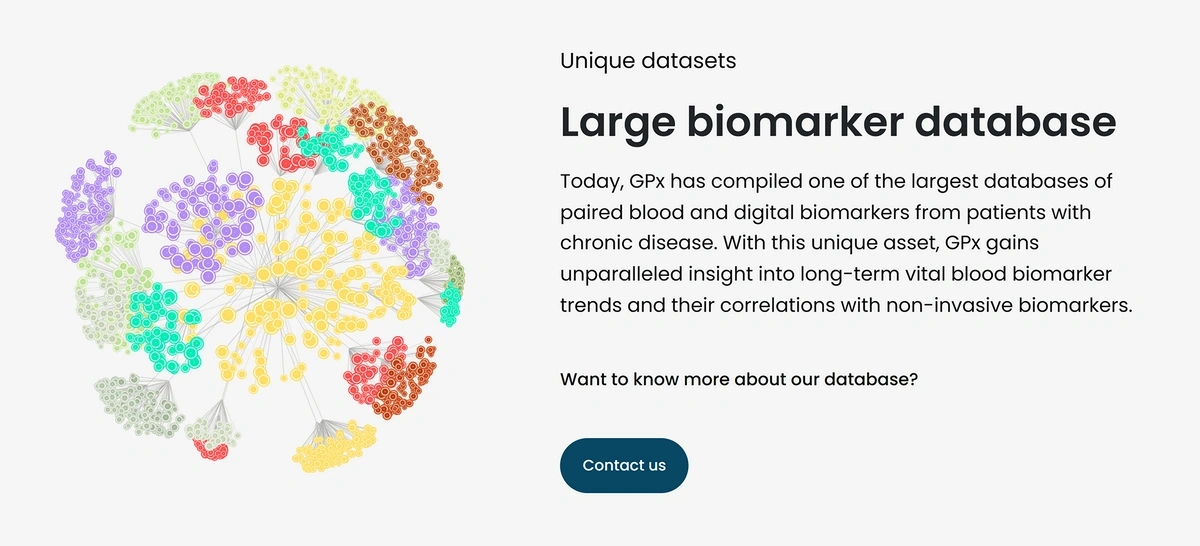
Another medical-grade wearable comes from GPx, a startup based in Boston.
“GPx” searches are up 45% in 5 years.
This device looks like a regular smartwatch, but the technology is much more sophisticated. GPx calls it Bloodless Blood Tests.
The smartwatch and corresponding app continuously and passively record biomarkers like heart rhythm, voice biomarkers, and activity levels.
Those biomarkers are fed into an AI platform that checks those factors against a database of blood biomarkers that were originally collected from heart failure sufferers.
The company’s expansive database enables them to run predictive algorithms for heart failure patients.
The algorithm can detect an increase in NT-proBNP (specific proteins linked to heart failure) up to 10 days earlier than traditional blood testing.
This device is still in the research and testing phase.
More than 113 million units of wearable technology were shipped in Q1 2024. Annual totals are expected to exceed 600 million by 2027.
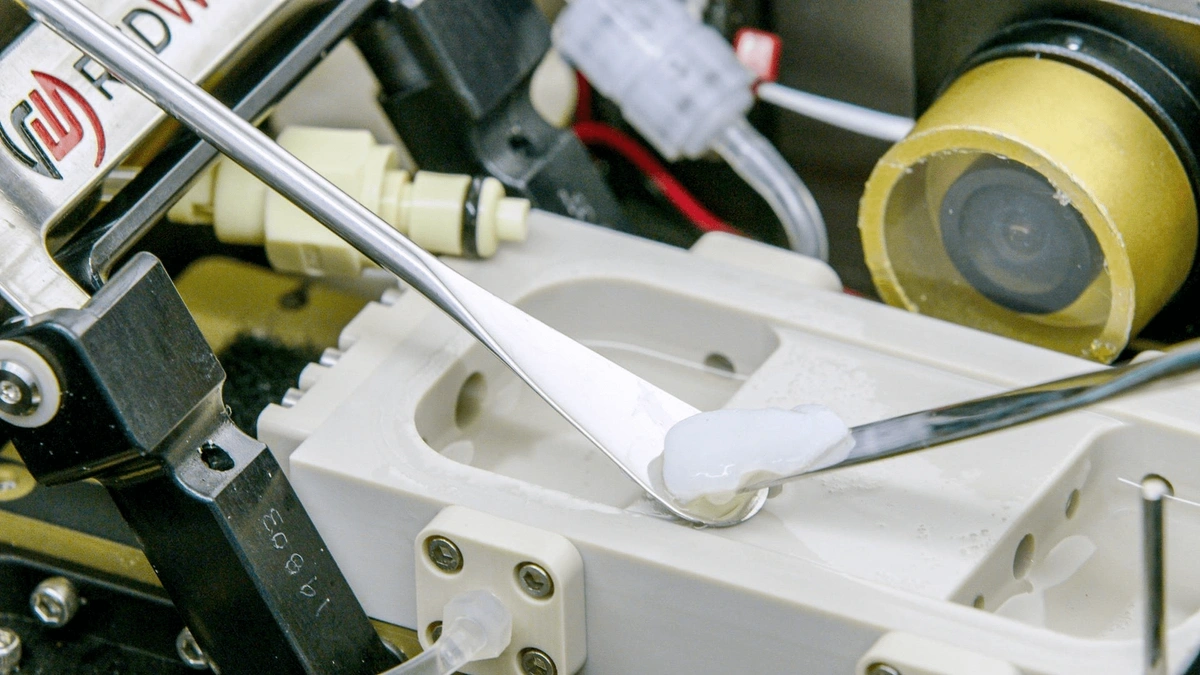
4. 3D Printing Makes Further Strides
Recent research and funding initiatives are driving the 3D printing market forward in the healthcare sector.
Estimates show the value of the market for 3D-printed medical devices could reach $16.5 billion by 2034.
There are numerous possibilities for 3D printing in the medical sector.
Consider 3D-printed anatomical models that can be useful for surgeons practicing procedures. Or specially-designed medical instruments and devices that can be 3D printed on-demand.
Some 3D printed materials are already being used to deliver personalized healthcare to patients, another big trend for the future of healthcare.
One example is 3D-printed joint replacements.
The Hospital for Special Surgery in New York has become the first in the US to house a 3D-printing facility onsite. It makes custom-made joint replacements for when “off-the-shelf” solutions won’t work.
It’s a collaboration with LimaCorporate, which was acquired by MedTech giant Enovis this year in a deal worth $800 million.
“Enovis” searches are up 8500% in 5 years.
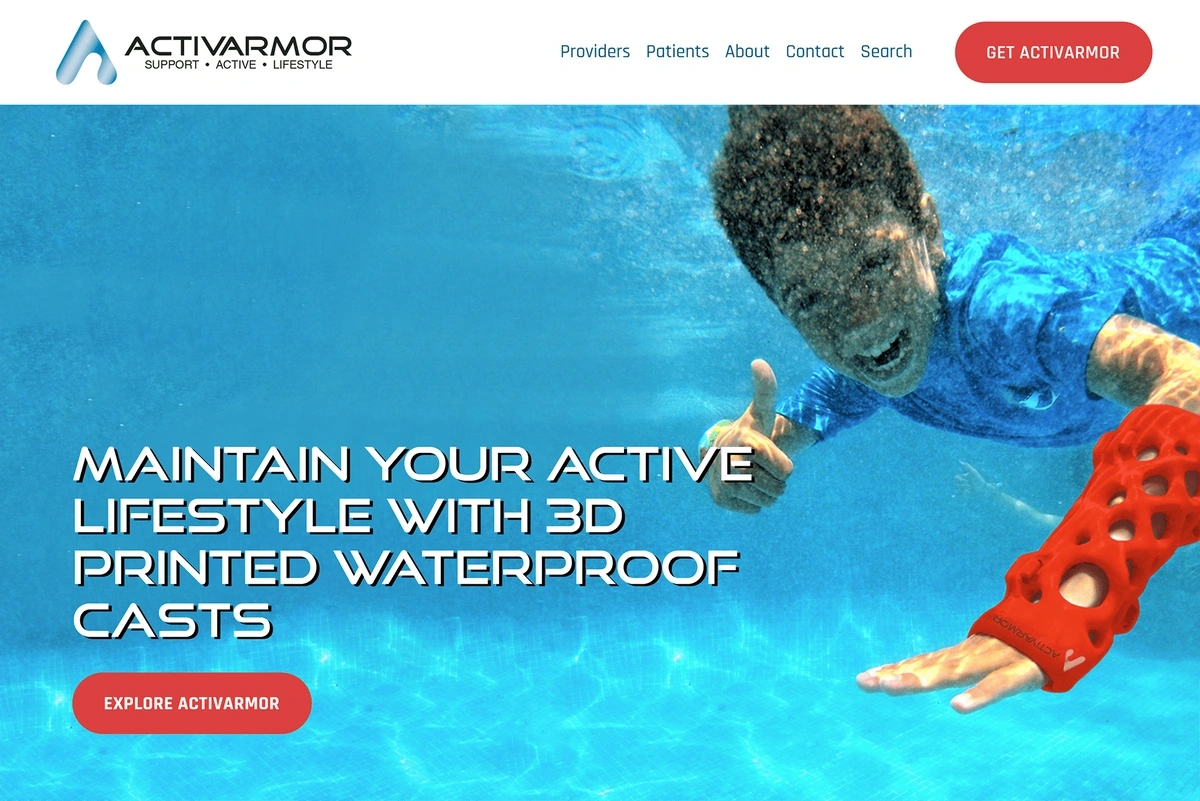
Meanwhile, 3D-printed casts are becoming more common. More than 100 doctors in the US have prescribed ActivArmor orthoses.
These casts are much more hygienic than traditional casts. They’re also lightweight and more durable.
Thanks to a 3D-printed cast, patients can take a shower and sweat all they want without worrying about skin irritation.
ActivArmor is the leading manufacturer of 3D-printed casts.
St. Luke’s University Health Network in Pennsylvania has installed an in-house ActivArmor printing lab, which expedites the process of getting the casts to patients.
Scans are taken on a smartphone. Those are converted into 3D-printing models, which can then be manufactured on site.
And the process of converting medical scans to 3D-printing data is getting more efficient. Axial3D uses AI to enhance the process.
“Axial 3D” searches are on the rise.
Medical scans are uploaded to the platform. The data is then segmented automatically, ready for 3D printing - although the end result is still verified by a (human) biomedical engineer.
Even with these remarkable advances in 3D printing, there’s still more to come.
Bioprinting is perhaps the most promising application of all.
“Bioprinting” is gradually moving from Sci-Fi to reality.
This is a type of 3D printing that uses biomaterials (living tissues) as the printing material.
Bioprinting experts hope that within the next 10 years, bioprinting will have “significantly reduced” animal testing, with drugs able to be tested directly on bioprinted organs.
And eventually, the goal is to be able to bioprint organs for transplant into humans.
Normally, these printing models require a “scaffold” to effectively encourage the tissues into growing in three dimensions. Surprisingly low-tech solutions have been pioneered, including hair gel and Jello.
But that’s not the case in space. NASA has astronauts working on bioprinting on the ISS, where the near-weightless environment allows tissues to grow in 3D without support.
A human knee meniscus successfully bioprinted using the BioFabrication Facility aboard the ISS.
Meniscus tears and other musculoskeletal complaints are among the most common injuries in the US military. Longer-term, NASA also hopes bioprinting could restore sight to the 30 million people with degenerative retinal diseases.
5. The Healthcare Disparity Challenge Is Taken Seriously
According to the World Economic Forum, healthcare access and healthcare outcomes vary significantly based on geography, race, wealth, educational level, and gender.
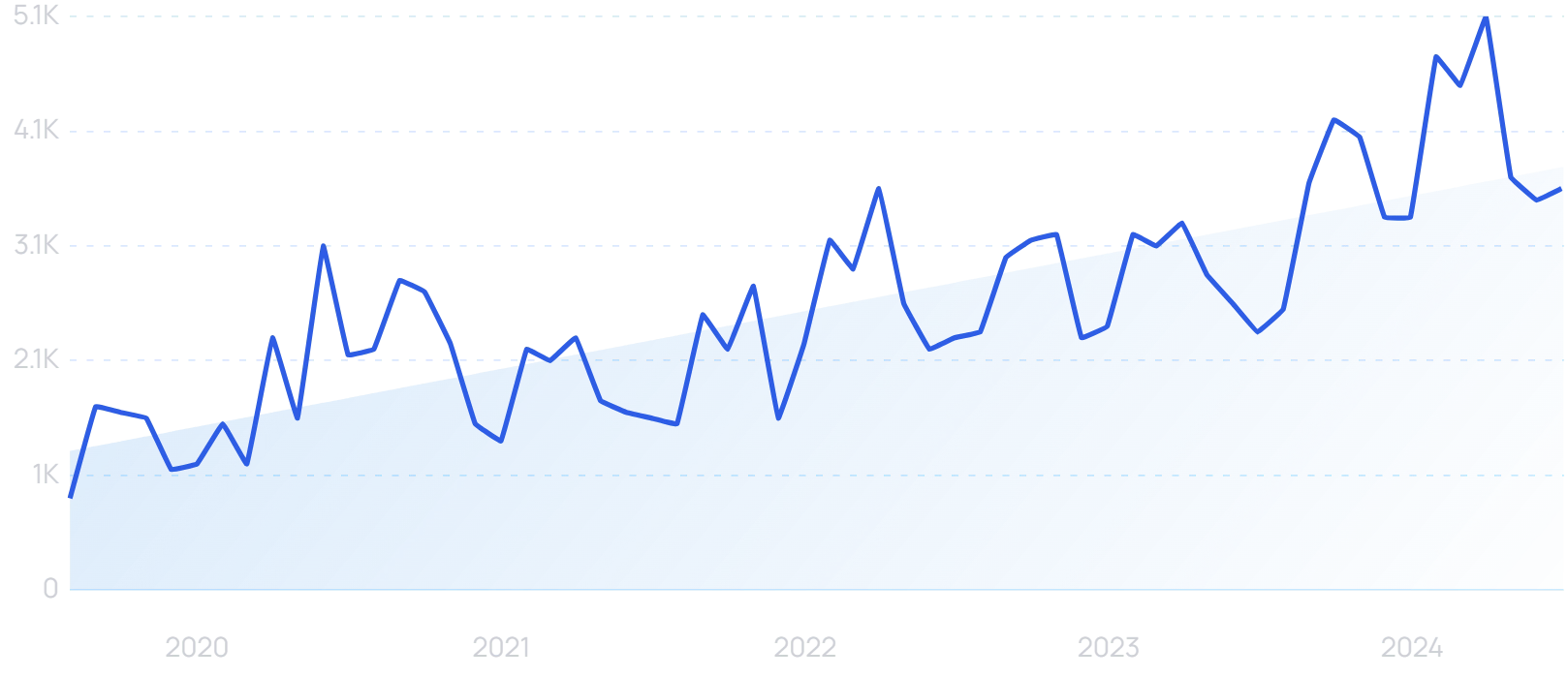
Search volume for “healthcare disparities” is up 338% in 5 years.
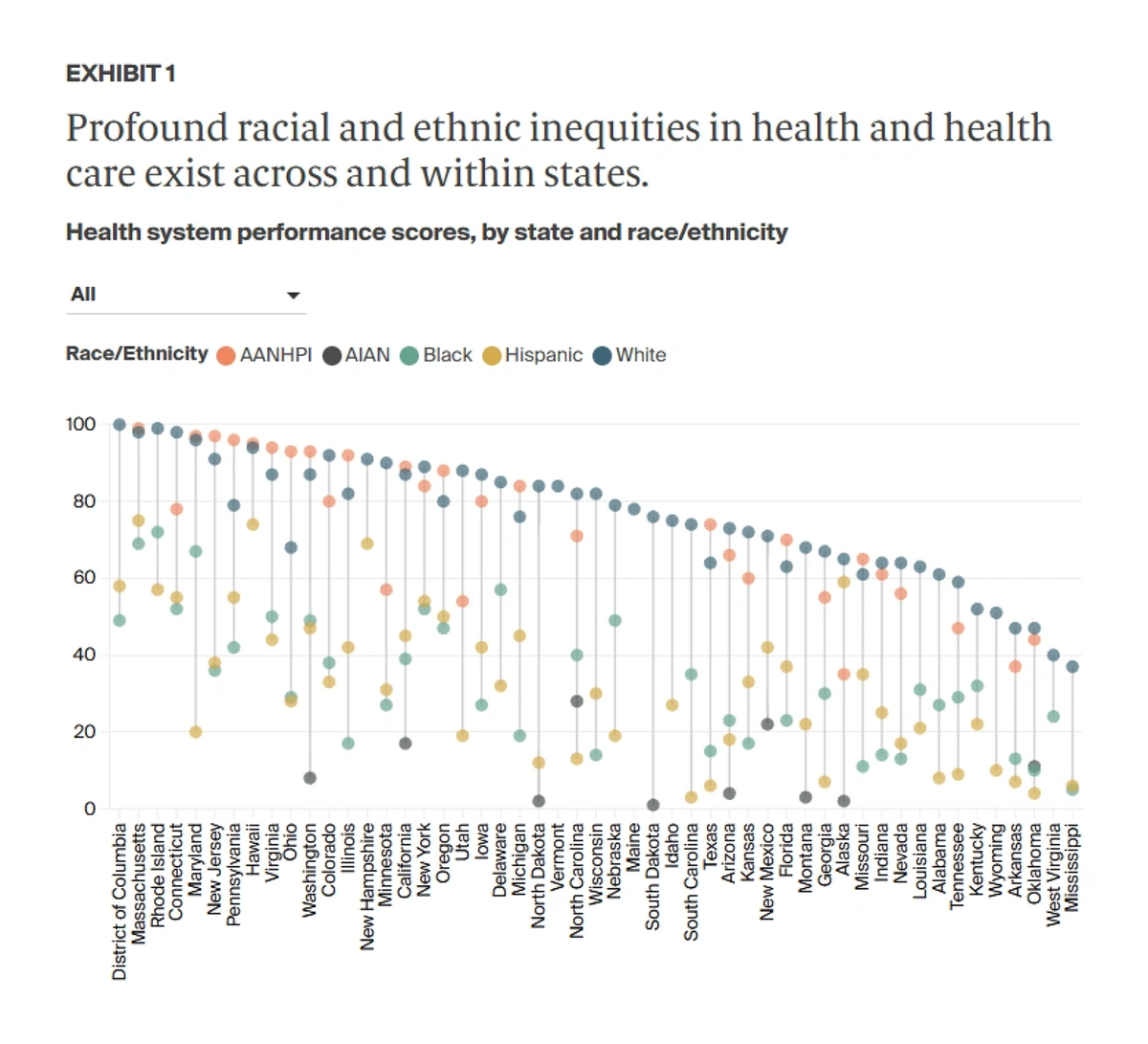
In the US, Black and AIAN (American Indian and Alaska Natives) people suffer far more preventable deaths than the White population.
The difference is most profound in South Dakota, where there are 1,394 preventable AIAN deaths per 100,000 population, compared to 252.6 preventable deaths per 100,000 among the White population.
The Commonwealth Fund’s 2024 State Health Disparities Report found White patients had the best outcomes in almost all states.
In another example, according to the latest World Health Organization data, almost 95% of all maternal deaths in pregnancy occurred in low and lower-middle income countries.
Minorities in the United States are also 2x as likely to be uninsured.
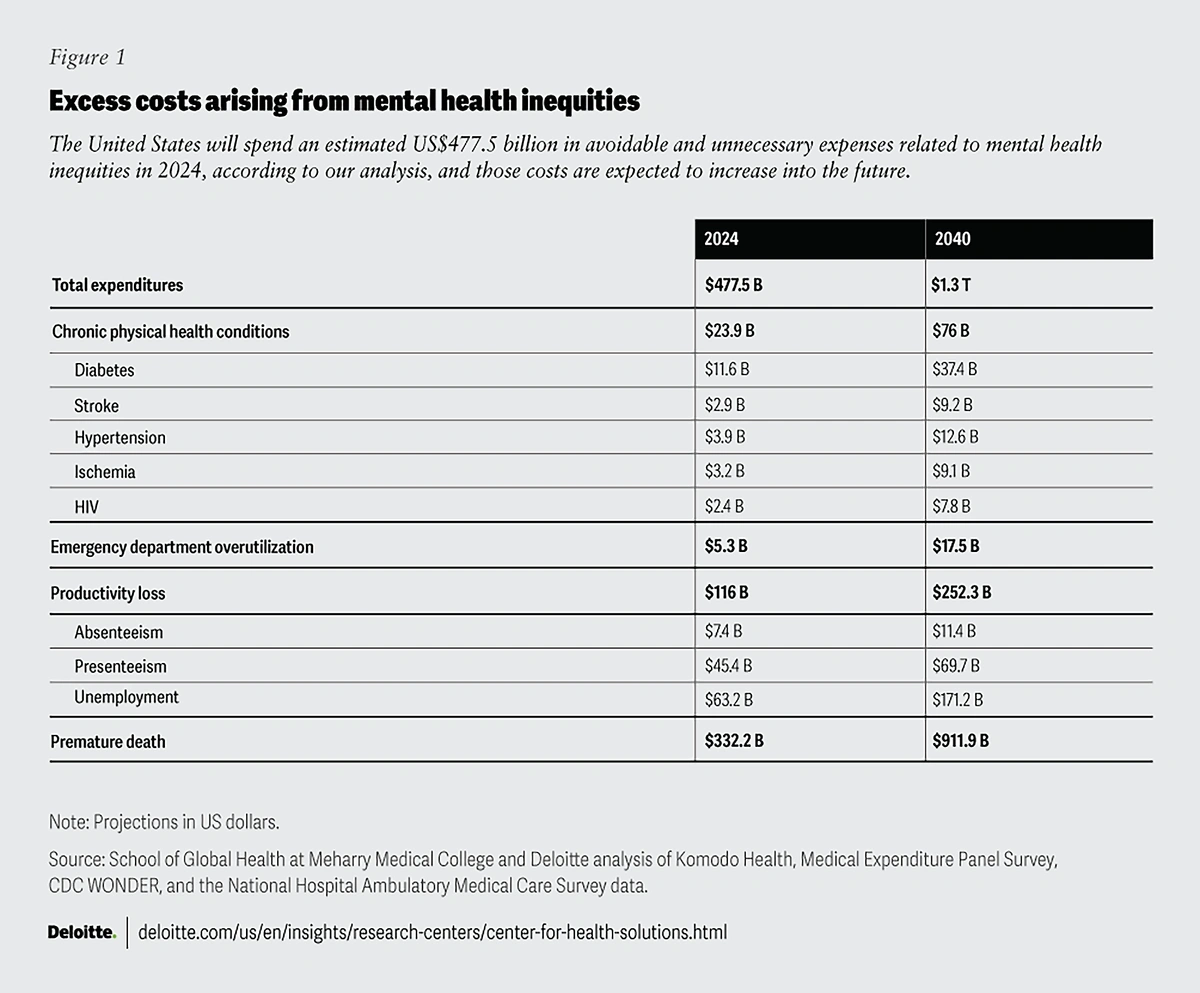
All of these issues are driving up costs. Deloitte estimates that in the US, the excess costs of mental health disparities alone could rise to $14 trillion between now and 2040.
This year, costs will total an estimated $477.5 billion. Premature death is the biggest cost to the economy, while productivity loss, emergency department overutilization and chronic physical health conditions are also factored in.
Failure to properly treat mental health issues among minority populations will cost the economy $116 billion this year in productivity loss alone.
Many groups and governmental agencies are beginning to call attention to the disparities in mental and physical health outcomes.
The US Department of Health has coordinated an initiative to end the heavily racially-skewed HIV epidemic, targeting a 90% reduction in new infections by 2030.
The Center for Disease Control has funded three research organizations in a bid to advance health equity in cancer treatments.
And the CDC also supports 44 states via the “ERASE” maternal mortality scheme. Black women are currently 3x more likely than White women to die from a pregnancy-related issue.
“Black maternal health” search interest is rising. Black Maternal Health Week takes place each April.
Private companies in the healthcare sector are also showing a commitment to addressing health disparities in the future.
Blue Cross Blue Shield of Massachusetts has launched a program to increase healthcare equity at hospitals and clinics.
The first participating organization is Tufts Medicine.
If the medical network can measure an existing baseline of inequality and prove they’ve created a reduction in that baseline, they’ll be awarded via a value-based payment structure.
“Value-Based Health Care” searches are up 8400% in 5 years.
For Tufts Medicine, the payments are specifically for reducing inequalities related to care for colorectal cancer, diabetes, hypertension, and well-visits for children.
Another innovation involves digital twins.
“Digital twin” searches are up 143% in 5 years.
Cleveland Clinic and MetroHealth have received a $3.14 million National Institutes of Health grant to create “Digital Twin Neighborhoods”.
Anonymized data from electronic health records is being used to create digital replicas of real communities served by the two organizations.
They should allow researchers to probe the health disparities within and between those communities, modeling ways to address them.
6. Healthcare Tackles Its Staffing Crisis
A shortage of 10 million workers by 2030 is projected within the healthcare sector.
And 87% of all US health care providers list staffing shortages as their biggest challenge.
Healthcare burnout is among the leading drivers of the staffing crisis.
“Healthcare burnout” searches have increased 152% in 5 years.
According to the CDC, 46% of healthcare workers “often” feel burned out. A similar number report intending to look for a new job.
In the last five years, the average hospital has turned over 106.6% of its workforce.
The most important solution is clearly to improve working conditions for those within the healthcare sector.
9 in 10 clinicians believe that involving frontline workers when developing programs to tackle burnout and staff shortages is an important step to take. But only 8% said that this happens regularly.
Alongside wellbeing improvements, healthcare organizations can also seek to utilize technology to streamline processes and free up time for clinicians.
More than 1 in 5 consultations in the US are remote. That figure rises to almost 1 in 3 in the UK.
“Remote healthcare” searches are up 471% in 5 years.
The benefits are often couched in terms of practicality for the patient. But almost half (45%) of clinicians across 11 developed countries also consider “improving my efficiency” as a major success factor of remote healthcare.
AI solutions can be an even bigger time-saver for healthcare workers.
One study found that the technology could save doctors and nurses an average of more than four hours of admin time per week.
Ada Healthcare is a medical chatbot. It provides a first point of call for symptom checks before a clinician needs to be engaged.
“Ada Healthcare” searches are on the rise.
The app has assessed more than 30 million symptoms. It has directed 40% of patients to lower-urgency care and reduced waiting times by 13%.
Conclusion
The future of healthcare is rooted in technology. The transformative power of data, devices, and AI has the potential to dramatically improve how medical systems operate and how patients receive care.
Personalized treatments and care are becoming a reality, but the privacy and security concerns surrounding this new way of healthcare will likely weigh heavy on the industry in the coming years.
Many in the industry are also paying closer attention to where these new advancements in care aren’t being realized.
Initial funding aimed specifically at underserved communities and populations has the potential to improve outcomes, but it’s clear that bridging the gap between communities and providers is a key step toward decreasing healthcare disparities.
Stop Guessing, Start Growing 🚀
Use real-time topic data to create content that resonates and brings results.
Exploding Topics is owned by Semrush. Our mission is to provide accurate data and expert insights on emerging trends. Unless otherwise noted, this page’s content was written by either an employee or a paid contractor of Semrush Inc.
Share
Newsletter Signup
By clicking “Subscribe” you agree to Semrush Privacy Policy and consent to Semrush using your contact data for newsletter purposes
Written By


Josh is the Co-Founder and CTO of Exploding Topics. Josh has led Exploding Topics product development from the first line of co... Read more